For most people, the link between the gut and our emotions isn’t an unfamiliar concept, from ‘gut feelings’ of apprehension to the gastrointestinal shenanigans that can come with anxiety. However, research in recent years suggests the link between the brain and the gut runs much deeper than that.
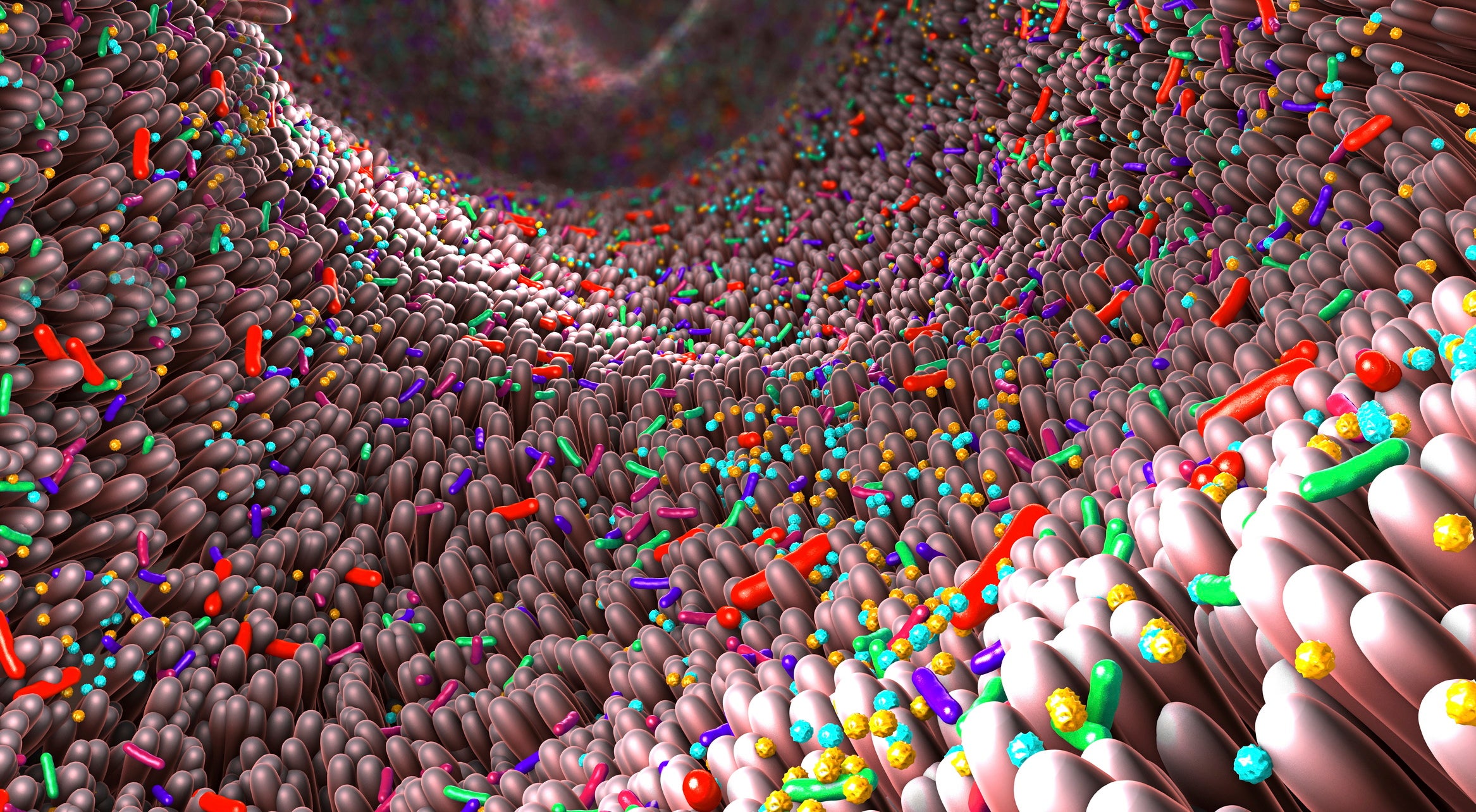
Research exploring this link has centred around the gut-brain axis, the bidirectional communication system between the brain’s central nervous system (CNS) and the enteric nervous system in the gastrointestinal (GI) tract. Signalling through the gut-brain axis is also thought to incorporate pathways including the CNS, neuroendocrine and neuroimmune systems, various constituents of the autonomic nervous system and the eco-system of micro-organisms that makes up the gut microbiota.
Where the gut goes, does the brain follow?
Scientific evidence is increasingly advancing theories that the composition of our gut flora could play an important role in the development of diseases and disorders, not only in the gut, but the brain as well, with neurological and neurodevelopmental conditions such as Parkinson’s disease and autism spectrum disorder (ASD) and mental health issues linked to potential communication between gut microbiota and the brain.
“We have seen there are a lot of changes in the gut microbiota, for example in patients with Parkinson’s or autism spectrum disorder, as well as depression,” says Dr Christine Fulling, senior research fellow at University College Cork’s APC Microbiome Institute, a leading global centre for research into the gut microbiome. “If we take the gut microbiota from patients with depression and transplant it to a mouse – or a rat in this case – we do see certain symptoms characteristic of depression in the rodent as well.”

The gut microbiome holds undeniable potential as a target for human medicine, and interventions based on manipulating the gut’s microbial population are already finding a growing role in healthcare, as APC Microbiome senior researcher Dr Maria Rodriguez Aburto notes.
“Faecal transplantation in humans has been proven to be very useful, for example in the treatment of Clostridium difficile infection, which causes very bad diarrhoea,” she says. “It’s very resistant to antibiotics, but faecal transplantation has proven to be very helpful. So we already have some very good cases for human application.”
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
By GlobalDataThe microbiome therapeutics market as a whole is seeing a surge of interest from drug developers and biotechs, with research from Polaris Market Research predicting a total market value of over $1.5bn by 2027. Indications attracting particular activity in the microbiome sphere include diabetes, various cancers and inflammatory bowel disease.
As for treating neurological and mental health disorders through the gut microbiome, that may be another matter entirely, as there are still some fundamental questions to answer about the complex link between the brain and gut.
The “magic and mysteries” of the gut microbiome
“We definitely still are at the tip of the iceberg,” says Fulling. “We do not really know the mechanisms. For Parkinson’s, for example, what is known is that there are changes in the gut at the very beginning of the disease – so are the changes we see for this disease actually the cause of the change in the gut microbiota, or is the change in the gut microbiota the cause for the onset of the gastrointestinal symptoms? There is a lot of evidence showing that the gut microbiota is in some part involved, but we still have a bit of the ‘chicken and egg’ problem.”
“It’s the big challenge in the field”, Aburto agrees. “To really understand how this communication happens, because it’s really complex. It involves a very complex community in the gut microbiome, which is not only bacteria but also viruses, fungi and archaea.”
As this field sits at the crossing between microbiology, pharmacology and nutrition, its study benefits from large, diverse teams, such as those at APC Microbiome, which can, as Aburto puts it, “look from different angles and understand this in a holistic way”. Even the institute’s own website refers to the “magic and mysteries” of the of the gut’s “bacterial community”, so taking a broad, multi-disciplinary approach meshes well with complexity of the scientific challenges ahead.
APC Microbiome’s staff of over 300 is split into four research themes, with one dedicated to the gut-brain axis. The researchers in this lab run a variety of projects to cover as many angles as possible across a range of model organisms, from how the gut microbiota of infants might be changed by their method of delivery to altering gut bacteria to work out how that alteration could be prevented in the future. Ultimately, Fulling says, the lab is pushing towards describing and explaining the exact mechanisms by which gut bacteria could communicate with the brain.
“There is the vagus nerve; there’s the immune system; there are hormones and neurotransmitters that can be released in the gut or actually by the gut microbiota, so that’s something we look at,” Fulling says. “At the end, we also look at very specific aspects, like whether specific neurons are changed, for example interneurons, or do we have microglia that are changed? Are there changes in permeability in the brain, in the gut?”
Potential therapeutic targets
With so many of the gut-brain axis’s mysteries still to be solved, clinical research related to the axis’s influence on neurological and mental health is thin on the ground, although some mixed results have been seen in clinical trials of certain GI-related targets. In ASD, for example, targeting the inhibitory neurotransmitter GABA – which is located in both the brain and throughout the GI tract – showed benefits in ASD symptom severity in a trial of generic edema drug bumetanide, although these benefits have proved difficult to replicate.
Aburto warns that further study will be needed before the clinical potential of GABA can be explored, but describes the neurotransmitter as an interesting approach to treating ASD’s inhibitory/excitatory imbalance, “because it could regulate that imbalance and ameliorate some of the symptoms”. Other avenues with potential for clinical development include the vagus nerve, the stimulation of which is already used as a treatment for depression, and short-chain fatty acids.

At the University of Surrey, an ongoing randomised clinical trial is investigating the benefits of prebiotic intake on the emotional regulation of 120 female participants aged 18-25. The trial, which is expected to complete in December this year, could form part of the pre-clinical evidence base for probiotic treatment of conditions such as major depressive disorder. The trial group’s age range is particularly relevant, as adolescence – along with infancy and childhood – represent key windows for gut microbiota interventions.
“When you’re born, you get your initial microbiota, but the gut microbiota doesn’t stay that way – it develops alongside the host until, in humans, around the beginning of adulthood, and then it’s more or less stable,” says Fulling. “But within this critical period that’s important for development, there’s also an instability within the gut microbiota, which can change drastically when there’s stress or something else.”
Several animal studies at APC Microbiome have centred on the effect of antibiotic and high-fat food intake, and found that changes to gut microbiota because of these inputs persisted well into adulthood. So could these semi-permanent changes to the gut microbiome ‘prime’ the gut bacteria’s composition for future responses to stress or anxiety?
“We didn’t test, for example, a ‘second hit’,” Fulling says. “What happens if now, the animal is stressed, how does the gut microbiota and the animal itself respond? It’s critical to know, because it might pre-set your gut microbiota for something that happens later in life.”
Gut-brain axis: the industry starts to take notice
With these sorts of open questions still on the table, it’s unsurprising that relatively few private pharma and biotech companies are willing to bet on developing transformative neurological and mental health treatments based on the gut microbiome. For university labs, funding long and complex pre-clinical studies can be a challenge, and investment is also needed to improve screening of clinically useful microbes.
“Right now, screening is very complex,” says Fulling. “It takes a lot of material and money, and we’re still not 100% sure what we need to know to understand whether we can go from the pre-clinical to the clinical model, and have a translatable effect there.”
As interest in the gut microbiome picks up, there is opportunity for collaboration with the pharma and food industries to support the fundamental science that could lead to therapeutic benefits. Such partnerships are common at APC, says Aburto.
“There is a symbiosis because both parties benefit from it. It gives the opportunity, if there is something interesting found in research, [to consider] how could this be commercialised or brought further in its clinical development? This is something that the pharmas can really help in bringing forward.”
And there are some early microbiome pioneers in the private R&D sector that have been looking to improve neurological therapies by harnessing the gut-brain axis. Boston-based Axial Biotherapeutics is a leader in the field; its drug candidate AB-2004 aims to reduce behavioural symptoms of ASD by removing certain autism-associated metabolites from the GI tract.
The company reported positive topline results from a Phase Ib/IIa trial in April, and expects to launch a Phase II trial before the end of 2020. Enterin, meanwhile, is progressing its lead compound, kenterin, which “improves neural signalling between the gut and the brain in pre-clinical models of Parkinson’s disease”, relieving the gastrointestinal symptoms that often accompany the condition.
While these companies and others are betting on the preclinical science translating into benefits for patients, the true therapeutic potential of the gut-brain axis can only be revealed when more of its mysteries have been solved – the communication routes between gut microbiota and the brain, as well as working out the cases when the gut microbiome is a cause of neurological and mental health conditions, rather than a symptom of them.
“We go back to the chicken and egg problem,” Fulling says. “We need to know what comes first to truly understand.”



