Despite the global disruption of the Covid-19 pandemic, the Nobel committees have still been awarding prizes for incredible breakthroughs and success in various fields.
While one committee awarded the 2020 Nobel Peace Prize to the United Nation’s World Food Programme, the medical committee decided to honour three scientists – Harvey Alter, Michael Houghton and Charles Rice – with the Nobel Prize for Medicine for discovering the Hepatitis C virus (HCV).
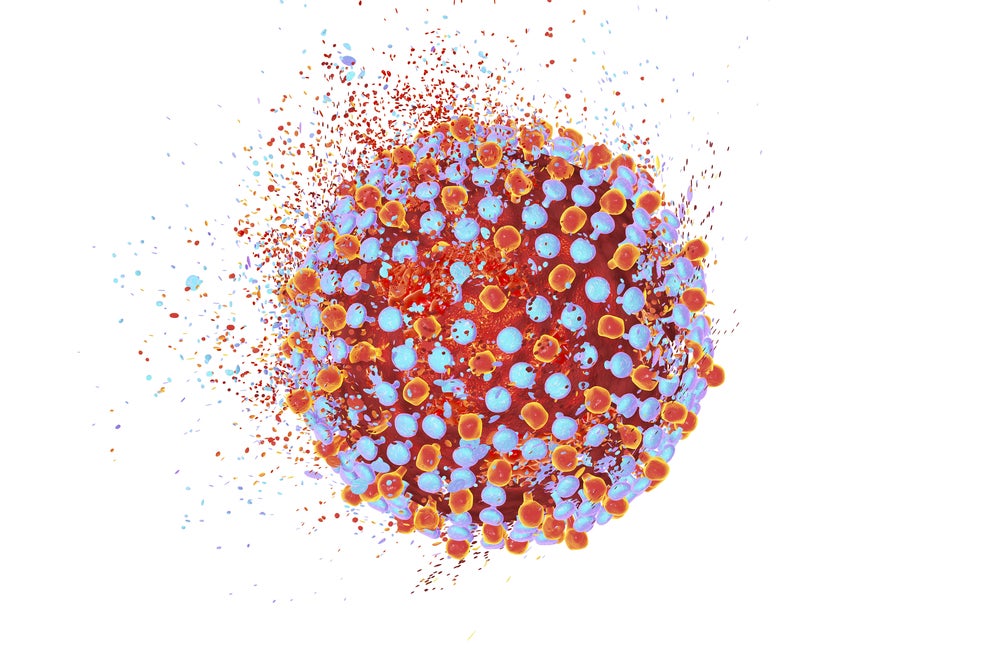
HCV is a small, enveloped, single-stranded RNA virus. Like human immunodeficiency virus (HIV), HCV is spread through blood-to-blood contact, including through injected drug use, poorly sterilised medical equipment and blood transfusions.
Otherwise known as inflammation of the liver, hepatitis is a puzzle that seriously challenged scientists. Despite the impressive discovery of Hepatitis A and Hepatitis B forms and associated viruses of the same name, many patients were still contracting hepatitis following blood transfusions, suggesting a third virus was at play. Hepatitis A virus (HAV) is transmitted through contaminated food, while Hepatitis B virus (HBV) is blood borne.
What was most concerning was this third type – which became known as HCV – was contracted through infected blood, exhibited little acute or short term symptoms that signalled a person had been infected and later caused serious chronic disease, and often then liver cirrhosis and liver cancer. The World Health Organization (WHO) estimates almost 400,000 people died as a result of the virus in 2016.
Therefore, understanding and identifying HCV was hugely important to combat hepatitis as a public health threat; studies suggest hepatitis is on par with HIV, malaria and tuberculosis in terms of global burden. The Nobel prize winning scientists’ work allowed for a fuller understanding of hepatitis, as well as the development of blood tests and new medicines that have saved countless lives.
How well do you really know your competitors?
Access the most comprehensive Company Profiles on the market, powered by GlobalData. Save hours of research. Gain competitive edge.

Thank you!
Your download email will arrive shortly
Not ready to buy yet? Download a free sample
We are confident about the unique quality of our Company Profiles. However, we want you to make the most beneficial decision for your business, so we offer a free sample that you can download by submitting the below form
By GlobalDataLet’s look back at the history of hepatitis and explore how these Nobel prize winning scientists solved the puzzle of HCV, therefore driving forward testing and treatment of this public health threat.
1800s – early 1900s: Jaundice and associated hepatitis kills soldiers in wars
Described by Hippocrates in around 400 BC, jaundice is the yellowing of the skin and whites of eyes. Hippocratic physicians then used this to link jaundice with the liver. It has since been connected with hepatitis as it is a clear symptom of a damaged liver.
As an infectious disease that is transmitted through contaminated food, water or blood, it is not surprising hepatitis and associated jaundice were rampant in the unsanitary conditions of the wars in the 19th and early 20th centuries.
It was particularly troublesome in the Second World War because soldiers were being vaccinated against other diseases and it was possible that these vaccines had been contaminated by hepatitis viruses. This led to localised epidemics, which have been estimated to have killed 16 million people.
1940s – 1960s: Emergence of two forms of hepatitis
Building on epidemiological studies into local epidemics in the late 1800s, in the 1940s studies were performed across Europe and in the US to find out how viral hepatitis is transmitted.
This led to Saul Krugman, who carried out experiments on mentally disabled children at the Willowbrook school in New York in the 1960s, to conclude there were two distinct forms of hepatitis. Although his methods were deemed unethical, he managed to show that the children were transmitting either HAV with a short incubation period or HBV with a longer one.
1960s: Discovery of HBV
In the 1960s, a geneticist at the US National Institutes of Health (NIH) Dr Baruch Blumberg began to collect blood samples to try and better understand the epidemiology of the disease and therefore prevent the spread. He noticed an unusual interaction between the serum of a haemophiliac who had undergone numerous blood transfusions and a protein in the blood of an Australian of indigenous descent. He named the protein the Australian antigen and, after further studies, he realised it was linked to viral hepatitis.
Simultaneously, research by Alfred Prince of the New York Blood Center used an immune-electrophoretic technique to identify a serum antigen associated with hepatitis. This antigen was later found to be identical the Australian antigen found by Blumberg.
Blumberg received the Nobel Prize for Medicine in 1976 for his description of HBV and his early work on a HBV vaccine. A more refined plasma-derived Hepatitis B vaccine was approved in 1981; it was manufactured by Merck and branded as Heptavax.
1970s: Identification of HAV
Research continued to try and understand hepatitis and the other strains that did not contain HBV antigens. The work by Fritz Deinhardt in Chicago and Stephen Finestone at the NIH were crucial in identifying HAV, which was causing short-term, acute hepatitis and was not transmitted through blood.
A vaccine for HAV was then quickly developed and approved in the 1990s; it was developed by SmithKline and branded as Havrix.
Late 1970s: Exploring a non-A and non-B form of hepatitis
Soon after the identification of HAV, US researchers, including Harvey Alter at the NIH, noticed the screening of donors for HBV prior to transfusions did not eliminate post-transfusion hepatitis cases. They also showed that these cases also did not have a HAV infection, meaning the post-transfusion cases had an unidentified cause.
There was some urgency to discover what was causing these post-transfusion cases given it was leading to chronic disease and cirrhosis much more often than HBV infection.
This new form of chronic hepatitis was named non-A, non-B hepatitis as it continued to elude scientists, including Alter, working on discovering the infectious agent causing it.
1970s – 1980s: Interferon emerges as a treatment
With HBV and HAV being identified and scientists continuing to search for the non-A, non-B hepatitis virus, other researchers got to work on finding treatments for hepatitis.
Studies showed that HBV patients responded well to interferon, a cytokine produced by the immune system against viral infections.
As a result, researchers at NIH did a pilot study of interferon against non-A, non-B hepatitis; the results were dramatic with 50% of patients showing no signs of liver infection in decade long follow ups. Interferon was approved for non-A, non-B hepatitis in 1984.
1980s: Discovery of HCV
In the 1980s, scientists working at California-based pharma company Chiron, including Michael Houghton, attempted to isolate the genetic sequence of non-A, non-B hepatitis virus in the blood of an infected chimpanzee. They utilised antibodies from the blood of patients with this type of hepatitis and searched for the same DNA fragments in the chimpanzee’s blood. In 1988, they found one positive clone and that it came from a novel RNA virus in the hepatitis family; they named it HCV.
However, this research was unable to show that virus was alone causing hepatitis. So Charles Rice at Washington University, St Louis, got to work and found a previously uncharacterised region in the end of the HCV genome. His research confirmed that the HCV alone was the non-A, non-B hepatitis virus.
1990s -2000s: New treatments emerge for hepatitis
As more and more studies were performed in HCV, interferon’s efficacy, particularly in the long run, was called in question. Therefore, the hunt was on to find new treatments for HCV, as well as other hepatitis viruses.
One early success story was ribavirin, a broad-spectrum antiviral medication effective for a range of RNA and DNA viruses. Although the rate of sustained virologic response (SVR) of ribavirin alone in HCV was disappointing, when combined with interferon, particularly a new and improved pegylated form, these drugs were highly effective at treating HCV. Pegylated interferon plus ribavirin was approved for use in 2001.
2010s: Enter DAAs
Importantly, the pharmaceutical research of the 1990s yielded further insights into the HCV’s biology and how it tries to evade treatment. This, and technical advances for improved drug screening, allowed for even better antivirals to be developed, including direct-acting antivirals (DAAs) developed specifically for HCV.
Researchers developed DAAs that targeted the HCV protease used for viral replication. These included telaprevir and boceprevir, which increased the SVR by 30% and were approved in 2011. Telaprevir was developed by Vertex and Johnson & Johnson, while boceprevir was developed by Merck.
Mid 2010s: Finding pan-genotypic DAAs
Unfortunately, many of the early iterations of DAAs – including telaprevir and boceprevir – were only effective in treating HCV genotype 1, whereas research around HCV tests and screening had showed that this virus has 6 different subtypes that determine its response to therapy.
Genotype 1 is the most common type in the developed world – particularly North America, Europe and Australia – whereas the other genotypes were more common in Africa and Asia. So, the next task was to find drugs to treat the other genotypes and resolve this public health threat on a global scale.
The result were pan-genotypic DAAs, which combine two DAAs together into a single pill – such as sofosbuvir and velpatasvir and glecaprevir and pibrentasvir. These therapies combined an NS5A inhibitor with either an NS5B or NS3/4A protease inhibitor to drive further efficacy at treating HCV, which had become very adept at developing resistance to earlier therapies. Combination therapies have similarly been very effective at keeping HIV and its drug resistance at bay.
As part of its 2017 plan to eliminate Hepatitis C by 2030, the WHO updated its guidance to recommend the use of pan-genotypic DAAs for all patients aged over 12. Historically, these drugs have been extremely expensive, but now generic versions are entering the market making them more accessible to those in need globally.
2020: Search for HCV vaccine
Despite the efficacy of DAAs against HCV, they cannot prevent people from getting infected with the virus, which is worry given symptoms are slow to develop, meaning transmission is hard to control. Therefore, it seems it will be extremely difficult to eradicate HCV entirely by 2030 without a vaccine. This is another way that HCV is similar to HIV.
Although HAV and HBV vaccines have been available and widely used for decades, it has proven extremely challenging to develop one for HCV. This is mainly linked to the number of genotypes of the virus and its ability to mutate, meaning it is difficult to induce an antibody response using vaccines.
However, researchers are starting to look at the possibility leveraging new vaccine technologies and developing DNA-based or virus-like particle vaccines against HCV.
For instance, in April 2020, scientists at Scripps Research designed an immune-stimulating particle that resembles a virus with modified versions of an HCV envelope protein to induce an antibody response in patients. Their plan now is to create a polyvalent vaccine that can confer protein against all six major genotypes of HCV. They are hoping to start studies in primates and human in the next year or so.



