
The 2015-2016 Zika virus epidemic has kicked off a global conversation over how best to diagnose, prevent and contain this new public health threat. At the peak of the outbreak, the vector-borne virus has wreaked havoc in countries with high populations of the Aedes genus of mosquitoes that spread it, bringing with it an unprecedented rise in infants born with microcephaly and other congenital brain abnormalities.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Outside of the many discussions related to mitigating future Zika outbreaks, the epidemic has also inspired some new scientific thinking. For Dr Harry Bulstrode, a clinician and scientist at the Cancer Research UK (CRUK) Cambridge Centre, Zika potentially presents a new method of treating glioblastoma, one of the most common and deadly forms of brain tumour. Even with top-of-the-line care, the majority of glioblastoma patients do not survive longer than a year.
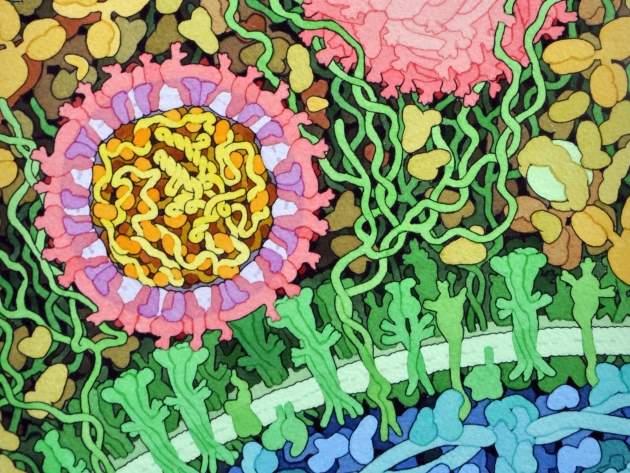
In response to this immense unmet clinical need in this field, CRUK in May provided a £200,000 grant under its Pioneer Award to Bulstrode to fund his team’s research into Zika’s potential as a glioblastoma treatment, or at least a route towards a therapy that can make use of its mechanisms. Researchers believe that the means by which Zika can pass through the blood-brain barrier and attack foetal neural stem cells could be harnessed to attack brain tumour cells, which resemble foetal neural stem cells. The virus’s relative harmlessness in adults is another characteristic that makes it promising from a therapeutic perspective.
“When the Zika epidemic came along, the more I read about it, the more it seemed to fit the bill of being an agent that was able to attack very specifically this foetal neural stem cell component, without having any great effect on adult brain tissue,” says Bulstrode. “So it seemed as though we had an interesting and important differential to investigate there.”
Here Bulstrode discusses this early-stage project, the potential benefits of Zika for glioblastoma patients and the risks and challenges involved in this pioneering research.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataChris Lo (CL): Why do you think Cancer Research UK committed to the £200,000 grant to fund this research through the Pioneer Award?
Dr Harry Bulstrode (HB): They [CRUK] have recognised brain cancer as a real priority area, because it is so poorly treated. I think, with that in mind, they’re looking for novel ideas that are nonetheless grounded in some solid science, and I think what they saw in this is that this is really a project based on and building on a lot of quite well-established stem cell biology.
Obviously it’s a bit of a stretch to think that Zika virus, as is, could be a useful adjuvant therapy. But even if Zika virus is not in itself a useful adjuvant therapy, we can learn a lot about ways of getting into the brain and ways of attacking specifically the stem cell population from this work.
CL: What has already been established about how Zika virus crosses the blood-brain barrier?
HB: Really very little. It’s not even so much that other viruses can’t cross the blood-brain barrier, and in actual fact there are already oncolytic virus therapy strands, so people have used modified polio virus and so on. But the problem with viruses like polio and measles is that if they get into the brain in their unattenuated form, they non-selectively attack all the cells and you get encephalitis and you get very severe illness in association with that.
What seems to be quite unique about Zika is that it tends not to cause any of that, but at the same time it is causing a very selective, devastating effect on the foetal neural stem cells. So crossing the blood-brain barrier is not unique for a virus, but crossing the blood-brain barrier and then specifically targeting this population that we’re after and doesn’t really perform much function in the adult brain – that is a special characteristic.
CL: What is it about Zika’s mechanisms that make you think it could attack glioblastoma cells?
HB: There’s a group at Cambridge, Fanni Gergely’s group at the CRUK Institute, who have been looking at the mechanisms by which Zika might be working, and they’re interested in its behaviour in development and in neural stem cells. It looks as though the RNA that encodes the Zika virus can fit into an RNA-binding protein that’s normally expressed in neural stem cells, and that’s fairly key to the division and proliferation of neural stem cells, and that’s called Musashi-1.
It looks as though Zika virus RNA can bind within the RNA-binding pocket of that protein, and in doing so inhibits the activity of that protein. So once in the cells where it finds high levels of Musashi-1, which are neural stem cells, Zika virus interferes with the function of the Musashi-1 and also ensures its own replication and ultimately the death of the cell.
CL: Would a therapeutic Zika-derived formulation need to be modified in some way to attack these cells, or could they attack the tumour cells naturally?
HB: Well in the simplest possible form, it’s not outrageous to suggest that you could just treat patients – post-surgical resection, you’ve got residual glioma stem cells in the surrounding brain around the surgical resection cavity, and let’s say a week post-resection, these patients could be admitted to an infectious disease ward and, under controlled circumstances, be infected with the Zika virus, and the virus would do what it has done to date in developing embryos and attack that cell population. That’s the most direct route.
From there, the model might be to think about modifying the virus. In actual fact, intuitively what most people who have some experience of oncolytic viruses are telling me is that probably Zika won’t be sufficiently aggressive in itself to do the job that we need it to. So it’s possible to add extra payload to the viral genome to make it effectively more tumour-ablative than even the wild type virus. That would obviously have safety implications as well, so that would need some very careful work.
And then the third line, which is probably the most promising, certainly from a pharmaceutical perspective, is you start to think about, ‘Right, how is this Musashi binding? How can we replicate this Musashi binding in a drug form, hopefully a drug that could cross the blood-brain barrier, and maybe we can use some of this specificity that Zika is demonstrating by replicating that Musashi-1 binding capacity.’ That would then need some medicinal chemistry and some other angles, but that would all be for a year or two down the line, once the basic stuff has been done.
CL: The virus itself is mostly harmless in developed brains, but are there still risks that need to be considered?
HB: David Rowitch, whose lab I’m working in at Cambridge, is quite anxious about this side of things because in the States – he works in San Francisco as well – when he started working with Zika, half of the post-docs in the adjacent lab walked out because they didn’t want to be in a lab where this virus was being handled, for obvious reasons.
But I think the more we understand about the virus and the transmission of the virus, the more it’s becoming clear that it needs category 2 safety precautions, which is how it’s classified, but it’s not transmitted in the absence of bodily fluid contact or in the absence of tropical mosquito vectors, so it’s relatively difficult to catch a Zika infection in an unintended fashion. So I think obviously we need precautions, but we’re not working with Ebola or anthrax here.
CL: At what stage is the research currently?
HB: We’re at a very early stage. I’m growing some cell cultures and just starting a first round of infection now. It’s awkward for me because I have a full-time medical job and this project is running alongside. I’m also in the process of recruiting staff for the lab bench side of things. It’s all getting going, but nothing is happening instantly.
CL: If all goes well, will you be looking to team up with a pharma or biotech partner to develop a commercial therapy?
HB: I think that would be one of the most exciting angles. Once we have an idea, which bits of the Zika programme are going to be useful therapeutically to start exploring avenues with a pharma company? Obviously oncolytic viruses are a bit of a niche to be in, but if we could start thinking about drug targeting of Musashi-1, for instance, that would be far more productive as a pharma problem, I suspect. That would be really exciting; essentially I’m going to need to find partners that have that interest and expertise, because it’s outside my domain.




