The etiology of both forms of inflammatory bowel disease (IBD), Crohn’s disease (CD) and ulcerative colitis (UC) is idiopathic, but to date physicians and researchers are still unaware about what causes IBD. According to epidemiological analysis from GlobalData’s Microbiome-Targeted Therapeutics in Immunology report, there are just over 4.7 million diagnosed prevalent cases of IBD in the 16MM. The Advances in Inflammatory Bowel Diseases (AIBD) Conference 2018 held in Orlando in December discussed possibilities of curing this chronic disease. However, since the cause is yet to be identified, is it too early to discuss methods of achieving curative therapies in IBD?
The short answer is no, although though the idiopathic nature of the disease makes it tougher to discuss about curative measures. The AIBD conference discussed the GEM study, which is a currently an ongoing initiative that has recruited patients with first degree relatives that suffer from CD; however, the participants themselves do not suffer from the disease. The aim is to monitor these patients and see if they would eventually suffer from the disease. To date, the study has recruited over 5000 participants in locations such as Canada, Israel, US, Sweden, and the UK. By monitoring their immune function, intestinal barrier and microbiome, clinicians hope to pinpoint the causes of CD for those who end up with the diagnosis. Learning about the changes in blood and tissue from those who eventually develop CD, physicians hope to gain greater knowledge about the disease and find ways of prevention by early medical intervention or accurate personalised treatment.
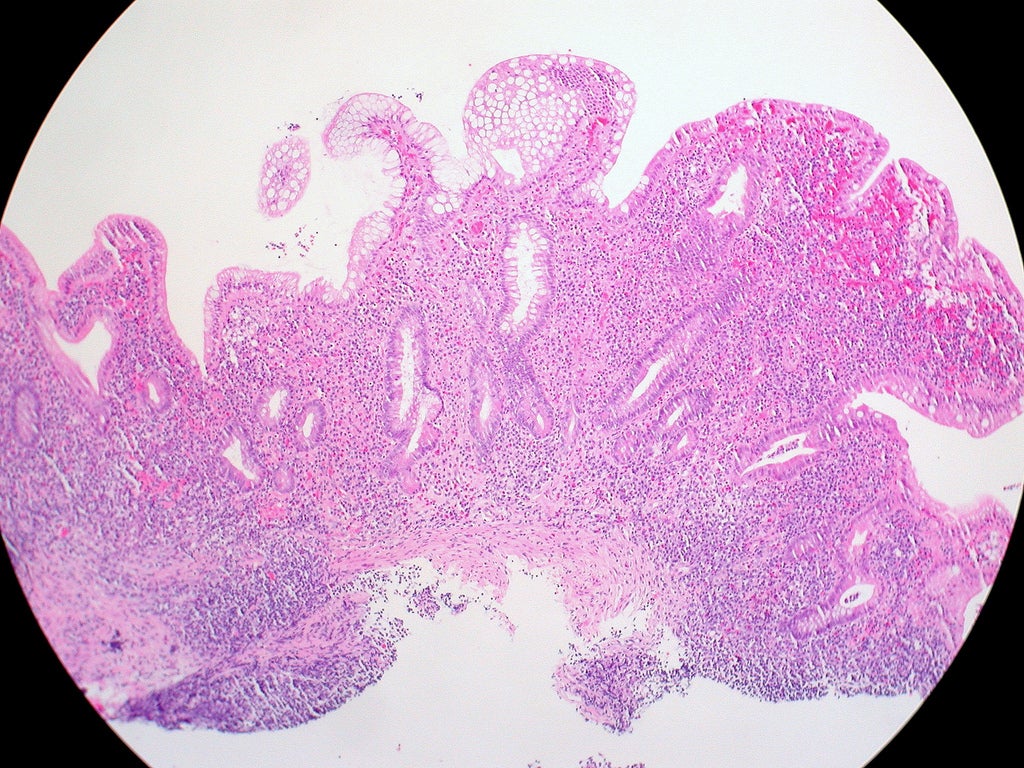
In addition to discovering the cause of the disease, it is also important to define the meaning of a cure. Besides prevention, another focus of discussion at the AIBD conference 2018 was how to limit patients to one flare in their lifetime. Although it is in very early stages, a two-pronged approach of targeting the host’s immune response and microbiome simultaneously was discussed. Immune response varies with each patient, it is also due to the immune response that IBD is caused. Furthermore, by looking into the biodiversity of the microbiome there may be a possibility of discovering whether a patient may develop the risk of relapse. Key opinion leaders (KOLs) interviewed by GlobalData have also suggested that early data has shown that patients with either UC or CD have a narrower diversity of organisms in the gut and patients who tend to develop IBD have different concentrations of different organisms. Conceptually by developing personalised approaches to deal with both and deploying it simultaneously, there could be a method of discovering a cure.
Currently many therapies that are developed for IBD are focused on one target, for example anti-interleukins and anti-TNF agents focus on specific cytokines. Researchers may need to look into the possibilities of treatments focusing on many different targets and different pathways. Currently Qu Biologics has taken the initiative to look at many pathways with the Phase IIb development QBECO-SSI for CD. In a Phase I/II trial in anti-TNF-naive patients, a statistically significant response rate, defined as a decrease in Crohn’s Disease Activity Index (CDAI) of ≥70 points, of 64% was observed in QBECO-treated patients at week 8 compared with 27% in the placebo control (p = 0.041). KOLs interviewed suggested that by focusing on different pathways it is possible to activate macrophages which will enhance immunity and could prevent the development of CD. Although it’s still in early stages, the possibility of having an IBD-free world without having complete knowledge of the cause could be possible in the foreseeable future.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData