At the 2025 European Association for the Study of Diabetes meeting in Vienna, University of Bremen investigators reported that microRNA‑155 (miR‑155) is significantly upregulated within the pancreas of donors with type 1 diabetes (T1D) and in autoantibody‑positive donors, while microRNA‑146b (miR‑146b) remains unchanged; the data suggest a pro‑inflammatory imbalance that could amplify local pancreatic inflammation and autoimmunity and may be therapeutically correctable.
T1D is an autoimmune disease where immune pathways drive beta‑cell stress and death, leading to loss of endogenous insulin and lifelong insulin therapy; microRNAs are small, non‑coding regulators of gene expression that modulate antiviral responses and immune activation, and shifts in their levels can tilt the balance between inflammatory drive and counter‑regulation in the islet microenvironment.
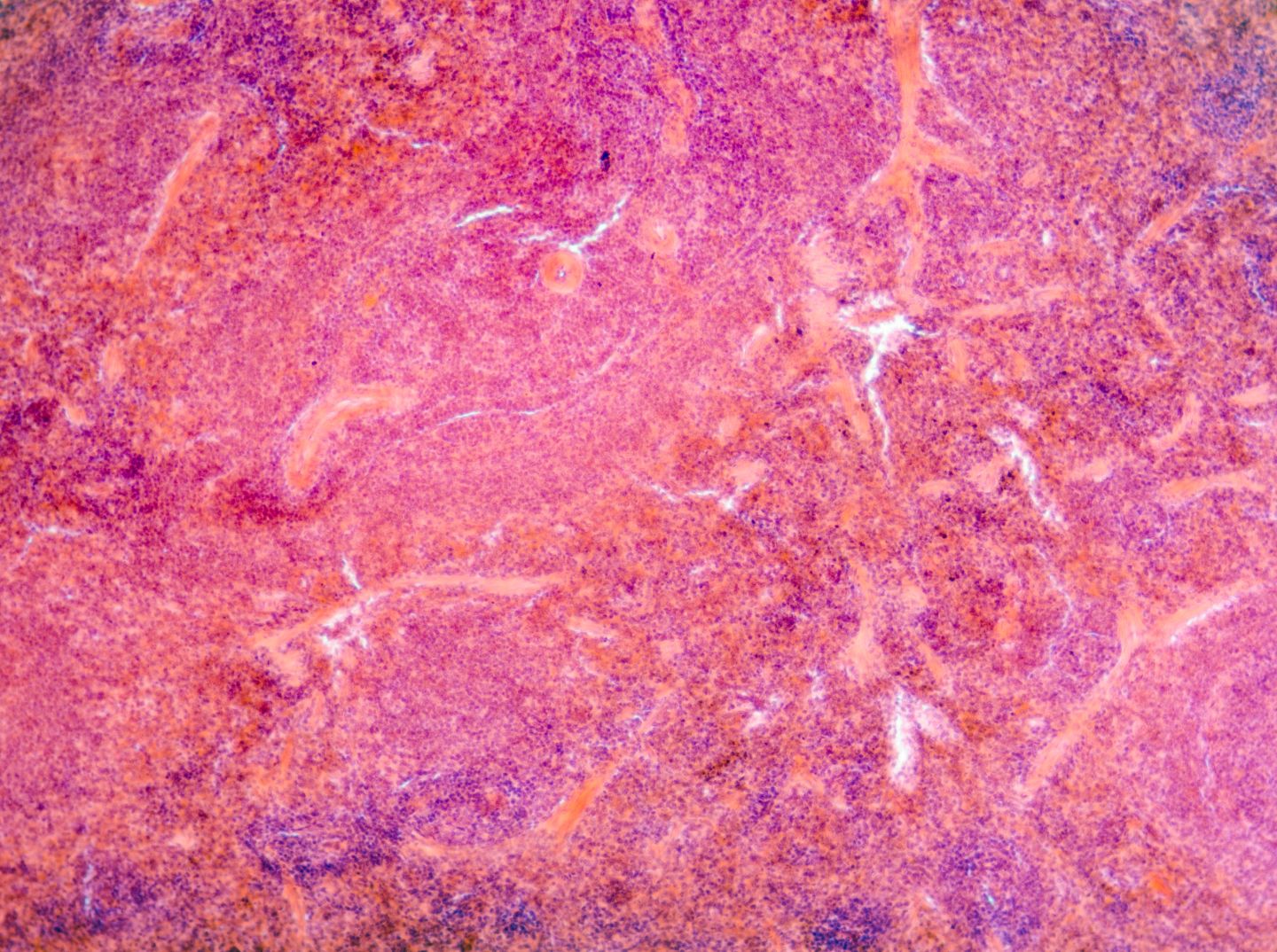
In human islets exposed to enteroviruses, both miR‑155 and miR‑146b rose in infected islets, and exosomes from infected beta cells carried higher amounts of these miRNAs to islets and monocytes, alongside induction of interferon response markers; the group optimised a combined immunohistochemistry and in situ hybridisation assay to directly localise miR‑155 and miR‑146b in formalin‑fixed pancreatic tissue, enabling spatial quantification.
Using this tissue‑level method, miR‑155 was significantly elevated in the exocrine pancreas of T1D and autoantibody‑positive donors compared with controls, while miR‑146b did not change across endocrine or exocrine compartments; stressors unrelated to cytokine or viral signals did not reproduce these shifts, indicating a disease‑relevant inflammatory and interferon‑linked signature rather than a generalised stress response.
Key opinion leaders (KOLs) interviewed by GlobalData said, “relieving patients of lifelong insulin is critical,” and pointed to the appeal of upstream levers that cool pancreatic inflammation without blunting insulin release; they viewed miRNA‑guided approaches to target inflammation at the source and reduce day‑to‑day management burden.
From a pharmaceutical strategy perspective, the findings elevate miR‑155 as a tissue‑level biomarker and potential target for early T1D intervention, opening avenues for antisense or miRNA‑modulating therapeutics and for companion diagnostics that stratify patients by pancreatic miRNA signatures; pairing transient interferon‑pathway inhibition with miR‑155‑focused modulation could offer a preservation‑first combination that is more precise than systemic immunosuppression.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataIf replicated prospectively, this tissue‑anchored miRNA signal could reshape the T1D treatment landscape by enabling earlier identification of pancreas‑active inflammation, guiding short‑course, biomarker‑timed therapy, and complementing beta‑cell preservation and restoration strategies, ultimately reducing reliance on lifelong insulin while maintaining functional insulin secretion.