Cardiovascular disease (CVD) includes any conditions that affect the heart or blood vessels. Treatment of this condition has largely been controlled by cardiologists, despite evidence suggesting that there are co-morbidities and cross-overs between CVD and inflammatory conditions. Targeting the inflammatory basis of the condition, rather than dealing with CVD symptoms, could be an effective, safe option for treating patients holistically.
US-based pharma company Abcentra wants to change this siloed approach to the benefit of patients. Former CEO and current senior advisor Bert Liang explains the company wants to create new therapies that target specific mechanisms of inflammation, making them stand out from broad, side effect-inducing biologics, for certain cardiovascular disorders, including accelerated atherosclerosis and aortic valve stenosis.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The company’s primary target is inflammatory mediator oxidised low-density lipoprotein (oxLDL) and its lead candidate is orticumab, the first fully human monoclonal antibody that targets this lipid.
Allie Nawrat: How is the current approach to treating CVD inadequate?
Bert Liang: One of the biggest challenges that we face with cardiovascular disease is the bleed over; what happens when you overlap with another therapeutic area? When you’re talking about diabetes, there’s a lot of integration between endocrinology and cardiology, but this does not happen with rheumatology and cardiology; people stay in their lane so to speak, and don’t look at the patient that is in front them. What we’re seeing is a lot of separation as a result, and therefore there’s not a lot of recommendations from the American Heart Association or the American College of Cardiology with regards to people who have rheumatologic disease and cardiovascular disease.
Patients with rheumatologic disease, like rheumatoid arthritis, psoriasis and lupus, all get atherosclerosis that is not only more frequent, but accelerated [compared to] the average person who doesn’t have those kinds of inflammatory diseases. The relationship between rheumatologic and cardiovascular disease is not new information – it was identified by the [1995] Framingham study in the US – but it needs to be studied more and we need to [find] a different approach going forward. As [currently] those particular rheumatology patients are at increased risk for cardiovascular events, but they are subject to what’s called secondary prevention, which is wait until they have a heart attack and then treat them. The problem is that half those patients could die [from] their first heart attack.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataAN: How is Abcentra attempting to change the CVD treatment paradigm?
BL: We have to break cardiologists and rheumatologists out of their own field and ask what is the best thing for the patient who is sitting in front of us and treat them accordingly.
At Abcentra, we are trying to change that by addressing specifically the inflammatory component of disease, so we can treat a patient’s psoriatic plaques as well as the other, cardiovascular parts of their inflammatory disease.
[We are building upon] one of the things that has happened more recently in cancer: approval of agents not on the basis of the location [of the tumour] or the indication, but on the basis of the pathway. I believe that focusing on the mechanism of the drug is the best way of doing it. Our target is oxLDL, which is an inflammatory mediator that’s been found to be more and more important over the past few years.In general, people are starting to realise that mechanism is important, and you shouldn’t stick to your therapeutic area. That being the case, things change slowly. We are going to be spending a lot of time proactively speaking with the regulators with regards to our product, only because they need to become more familiar with the fact that we’re playing in areas of the overlap.
AN: What makes oxLDL an effective inflammatory target in CVD?
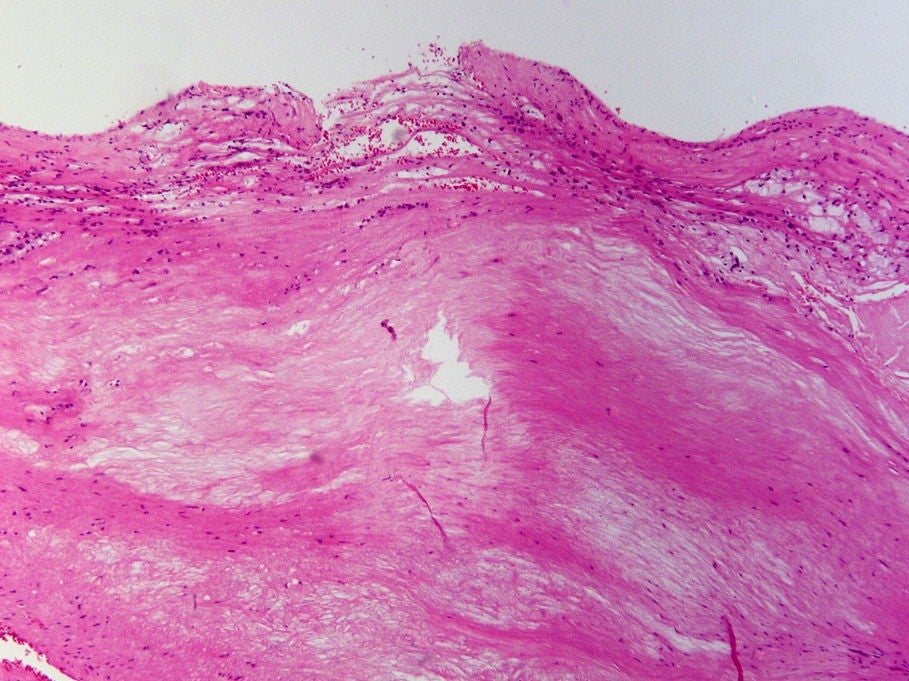
BL: Interestingly enough oxLDL is an older target. Two of the founders of our company, Prediman K Shah at Cedars Sinai Medical Centre in Los Angeles and Jan Nilsson at the University of Lund [in Sweden] have been studying the target for over a decade, and they knew that oxLDL was an inflammatory mediator of cardiovascular disease. If you start looking back in the literature, what you see is that in fact, oxLDL was also one of the first inflammatory mediators noted in rheumatoid diseases; it was found in the joints of the patients with rheumatoid arthritis and found in the skin plaques of patients with psoriatic disease. The target is interesting because of its inflammatory mediated mechanism.
It differs from the powerful anti-inflammatory biologics out there; yes, they can decrease inflammation, but they may actually be causing considerable issues going forward, such as increased infection and cancer incidence, as well as higher death rates. Instead, by being specific in the select mechanism with oxLDL, we’ve not gotten those kinds of side effects in about 250 patients.
This is why we are focusing on selective areas where we see oxLDL as a potent inflammatory mediator and we are just addressing these. I can’t say ox LDL is the inflammatory mediator for all inflammatory diseases, but it has proven to be effective in accelerated atherosclerosis and I think aortic valve stenosis is going to be an important component of our future studies.
AN: What are the next steps for your portfolio of oxLDL-targeting drugs?
BL: There’s a number of different areas that have been shown to be important with regards to oxidised LDL. It has at least two mechanisms of action, the first is that it causes the release of a certain kinds of cytokines that promote inflammation, and then it also binds to certain receptors that also increase inflammation.
Some of those receptors are present in cancer cells, and as a result, potentially being able to block that will be something that would be very interesting going forward for us to try to evaluate looking at these various types of mechanisms in other therapeutic areas. What we’re trying to do going forward is really look to see where the mechanism takes us.




