Cancer is an incredibly difficult disease to treat with even the most advanced drugs in the field only reaching the target tissue less than 1% of the time. Researchers are hopeful that a new method will – quite literally – shed some light on the situation. They’re using optical microscopy to map for the first time the journey of nanomedicines from delivery to final destination and the hurdles tripping them up along the way.
Targeting the cancer within tumours is an extraordinarily complex process. Not only do tumours vary depending on the type of cancer, each and every tumour within the same sort of cancer is unique and even within the same tumour, drugs are only able to reach certain areas depending on the way the cells are organised.
This goes even for the most advanced cancer drugs available today – targeted nanomedicines – which are specifically designed to deliver treatment to precise areas of the body. Meta-analysis carried out at the University of Toronto (U of T) has found that more than 99% never reach their intended destination, the result of the multitude of barriers they have to overcome, including specialised cells in the liver designed to destroy them (80%-95% don’t make it past this point) and various components within the tumour itself working to prevent take-up by cancerous cells.
Spotlight on nanoparticles
Aware of the existence of these barriers but still unsure about exactly how they work and how much they contribute to nanoparticles’ more than 99% failure rate to reach cancer cells, a team of scientists at the U of T’s Institute of Biomaterials & Biomedical Engineering (IBBME) decided to investigate.
Using a method developed at Stanford University in 2013 called CLARITY, which was originally designed to render mouse brains transparent, they have developed an optical microscopy technology through which they can watch nanoparticles journey from delivery to tumour, in the process finding out precisely where they’re gathering and what’s hindering their progress.
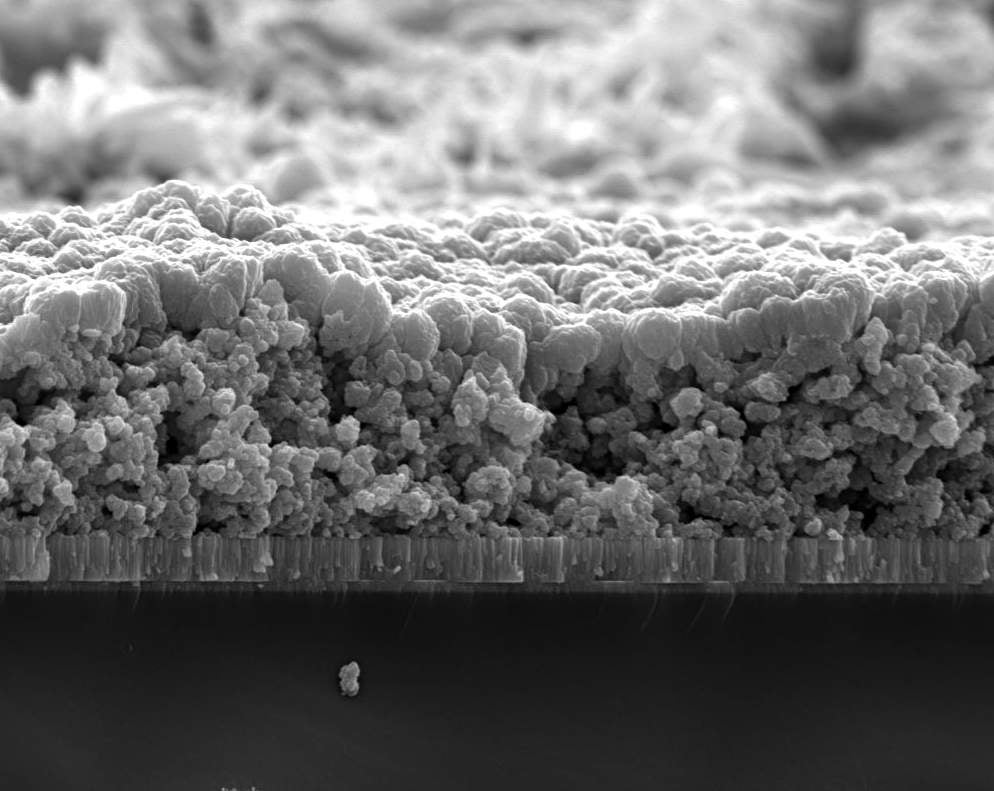
“Basically, we cut out the tumour, make it optically transparent using chemical procedures and then we can visualise the nanoparticles inside the tissue,” explains Stefan Wilhelm, lead author of the original nanoparticle meta-analysis.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalData“It’s like a freeze frame within a video game,” adds Abdullah Syed, a PhD candidate working on the project. “The nanoparticles look like points of light arranged in a random way, but if you think of it as a building, you can see that there are more in some rooms and on some floors.”
If you then repeat the process at several different points in time, the idea is that the points of light will have moved to different places, allowing the researchers to infer which areas the nanoparticles could move through with ease and where they got stuck.
“We want to understand what each of the barriers are doing and figure out how much each of those barriers contribute towards nanoparticles not getting to cancer cells,” says Shrey Sindhwani, another PhD candidate at IBBME.
Of course, all of this is done at an unimaginably tiny scale. “We knew that the CLARITY technique could analyse large volumes of data and tumours are a perfect candidate for large volume analysis as they are so complex,” Sindhwani says. “Using the technology, we can visualise single nanoparticles within the tumour, which are about one-thousandth the width of a human hair.”
A mathematical model for tumours
At present, the team is in the process of analysing the thousands of images they’ve collected so far. The ultimate goal is to come up with a mathematical model that quantifies exactly how the various barriers within the body prevent nanoparticles from reaching cancer cells.
“It would be similar to the way we have parameters for the functioning of the heart,” Sindhwani explains. “You can measure the blood pressure, you can tell when the heart is working normally and when it isn’t. But we don’t have this kind of understanding of tumours yet. We don’t have any parameters to assess whether a particular nanomedicine will work or not work with a particular kind of tumour.”
Once created, this predictive model could be used for characterising and cataloguing various different types of tumours. “We could then start screening different types of nanoparticles and trying to match them to a particular tumour type,” explains Sindhwani. “That way, doctors could select a particle type based on the architecture and biology of the tumour of each particular patient – they’d be able to figure out what drug or drug type would be the best way of treating that person.”
Wide applications
The applications of optical microscopy go far further than personalised treatment of tumours. As Wilhelm explains: “A good analogy for the technology is Google – it has a map of the world and you can zoom into different locations you’re interested in.”
With CLARITY, you could potentially do this for any organ. The technology was initially developed to map the brain, but it could ultimately be used to generate a map of any organ in sub-cellular resolution and visualise and quantify the interaction of nanoparticles within it.
“Basically as long as you have a disease in mind and a biological question you need answering, it can be applied,” Sindhwani says.



