Many pharmaceutical and biotech companies are finding that the economic tide of drug development has begun to turn against them. The arduous and costly process of developing a new drug for approval by the US Food and Drug Administration or the European Medicines Agency is increasingly discouraging investment in new therapies, leading to a clear lack of innovative new medicines in recent years.
Imaging biomarkers, used in clinical trials to detect and predict early responses to new treatments using imaging technologies, are being hailed as an important part of the struggle to control costs and streamline the clinical trial process.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The potential for these biomarkers to give drug developers important early information on the efficacy of a new therapy is impressive, but these early ‘surrogate endpoints’ can be misleading if not analysed properly, as they do not necessarily correlate with longer-term endpoints like mortality and morbidity.
Nevertheless, imaging biomarkers are gaining more traction in the drug development world, especially in the fields of oncology, neurology and cardiology, and should continue to do so as technology and techniques improve.
The US-based Clinical Trials Network (CTN) was formed by the Society of Nuclear Medicine in 2008 to advance the use of molecular imaging biomarkers in clinical trials. We talked to CTN chairman and University of Iowa director of nuclear medicine Dr Michael Graham about the advantages and pitfalls of imaging biomarkers, and what steps need to be taken to see this technology become a larger part of clinical trials in the future.
Chris Lo: Could you give a brief introduction to imaging biomarkers and their usefulness in drug development and clinical trials?
Dr Michael Graham: The major use of biomarkers in clinical trials is to establish early response to therapy.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe concept is that after a very short course of therapy, we should be able to see physiologic or molecular changes in the tumour that would precede any shrinkage of the tumour by weeks or even months.
CL: In what clinical development areas have imaging biomarkers been particularly useful in recent years?
MG: They’re useful in other settings, but not particularly in assessing response to therapy. In cardiac imaging, there’s been recent use with MIBG [metaiodobenzylguanidine] for predicting arrhythmias.
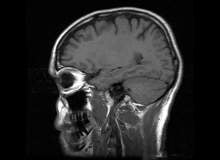
In the brain, we use some agents to look at dopamine activity in the basal ganglia to assess movement disorders and help diagnose which movement disorder it is.
It’s particularly useful in early Parkinsonism. Generally, the three major areas in molecular imaging and in nuclear medicine in general are cardiology, neurology and oncology.
CL: In these areas, do biomarkers have the potential to speed up the drug development process?
MG: In a number of different instances, yes that’s true.
In the brain in particular, there’s a lot of effort right now to develop and obtain approval for the amaloid imaging agents as a way to assess people with dementia, particularly those with Alzheimer’s.
The reason for the enthusiasm there is that such agents are going to be necessary to adequately assess the anti-amaloid therapies.
You can’t effectively develop those therapies unless you have some way to monitor what’s going on, and you can’t develop the amaloid imaging agents unless there’s a need for them. So there’s a chicken/egg problem that has slowed development for years.
CL: What is the main priority of the Clinical Trials Network in advancing this technology?
MG: Our primary priority is standardisation. We were concerned that there had been a number of clinical trials that had been done using imaging biomarkers, and in particular nuclear medicine agents, that had been done poorly, and as much as 40% of the data was unusable at the time of the final analysis.
This is a source of embarrassment for the people that practice nuclear medicine, and it’s a huge source of annoyance to the companies that use these biomarkers in their clinical trials.
And it was largely because of a lack of standardisation and understanding how to do these studies in a reproducible fashion. So that’s our primary emphasis, to make sure that the sites are capable of doing the studies and understand the importance of doing them in a consistent fashion.
CL: The risk seems to lie in setting surrogate clinical endpoints using biomarkers that don’t correlate with long-term endpoints. Is this still a problem, and can biomarkers become as reliable a part of clinical trials as anything else?
MG: I think they can, but the trouble is that there are a lot of variables in doing these studies properly, on the technical side, on the data analysis side, and on the imagery construction side.
There are several different points in the sequence where things can go wrong. But if it’s done consistently I think it should be reliable.
There’s an unfortunate tendency in our specialty to say ‘Well, I think it would be better if we tweaked this or if we imaged a little later or earlier’. And that just invalidates our whole ability to compare one site with another.
CL: How can using imaging biomarkers make the drug development process quicker and more effective?
MG: The agent that we have been focussing on is fluorothymidine (FLT), and that’s a marker of DNA synthetic rate. There are a number of examples in the literature, where it shows quite clearly that at one week after beginning therapy, there’s a marked change in the fluorothymidine uptake in the tumours.
Furthermore, you can use it to distinguish people who are going to respond from those who are not going to respond.
It’s getting to the point – and this is where we’re not quite there yet, it isn’t a validated biomarker but the evidence is accumulating that if you see no change in the FLT uptake at one week into therapy in most tumours and most drugs, it suggests it’s not an effective agent.
We have to continue to collect data to be able to make that statement even more strongly, but the evidence is building up that this is going to be a very important use.
For the pharmaceutical manufacturers, it’s going to make them ask if it’s worth going forward with a particular drug if there’s no effect as measured by the FLT.
CL: Do you think these sorts of biomarkers will give pharmaceutical companies early warning about whether to continue developing a particular drug?
MG: Yes; I kind of doubt that it would be the only piece of evidence they would look at in making that decision, but it would certainly be a very important piece. This go / no-go decision is a critical one that they need to make as early and as accurately as possible.
CL: Are biomarkers seen as complementary to more traditional endpoints, or as a potential replacement?
MG: At the moment, I think they’re complementary. I don’t think we have sufficient evidence to suggest we’re in a position to replace all the other methods. But as the evidence and performance accumulates, I think they will become more and more important, and ultimately they could be the primary determinant.
CL: What steps need to be taken to make imaging biomarkers a bigger part of the drug development process in the future?
MG: I think there needs to be collaboration between the industry, academics and the FDA, because the regulatory burden slows things down enormously.
I think there needs to be strong communication between pharma and the academic world to really make this work well in the future. In a sense, the academic community has the tools and the capability to come up with answers to questions, but we don’t have the questions. Pharma clearly has the problems and the questions that we need to assist with, so we have to work together so that we’re pointed in the right direction.




