HeLa cells are the most widely used human cell line in biological research, and for almost 70 years they have played a central role in many of mankind’s most significant biomedical breakthroughs – the cells were used in 1954 to develop the polio vaccine, in the 1980s to identify and understand the human immunodeficiency virus (HIV) and even in research for vaccines against Covid-19.
HeLa cells have formed the foundation of clinical trials to treat and cure cancer, contributed to space travel research and allowed researchers to identify the number of human chromosomes. They’ve helped develop treatments for Parkinson’s disease and haemophilia, establish methods of freezing cells for storage and discover the telomerase enzyme that contributes to aging and death.
But the story behind these cells is one steeped in racial inequality. The name HeLa refers to the initials of Henrietta Lacks, a poor, Black woman who died of cervical cancer aged 31 in 1951. While diagnosing her disease, doctors at Baltimore’s Johns Hopkins Hospital gave a biopsy of her cancerous cells to Dr George Otto Gey, a cell biologist based at the hospital’s medical school.
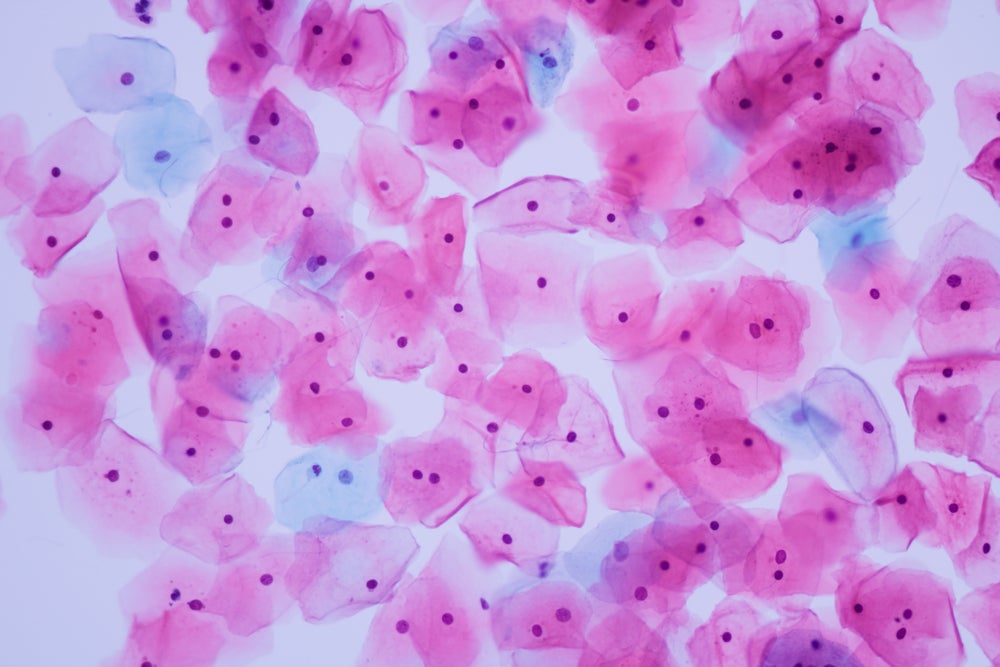
Lacks’ cancer was a uniquely aggressive case, and her biopsy sample doubled in volume every 20 to 24 hours where other cultures would normally die out. If they were fed the right mixture of nutrients to allow them to grow, the cells were effectively immortal.
We still don’t fully understand what made them so special, but it was likely a combination of the aggressiveness of her cancer, the cells having multiple copies of the human papillomavirus (HPV) genome and the fact that Lacks had syphilis, which would have weakened her immune system and allowed the cancer to spread further.
Gey later propagated the cells to create the HeLa cell line and made them freely available to other researchers. The cells were later commercialised but have never been patented.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataNeither Lacks nor her family gave permission for the cells to be harvested, something that was neither required nor commonly sought at the time – and still isn’t. While the multibillion-dollar biotech industry was built on the back of the HeLa cells, her descendants received no financial compensation and were not consulted in the projects in which they were used.
Science writer and Henrietta Lacks Foundation board member Dr David Kroll puts it into perspective: “Members of the Lacks family were having all this medical research done on their matriarch’s cells, but they couldn’t afford healthcare themselves.”
Reparations are opening up new conversations
Established by Rebecca Skloot, a science writer whose 2010 book The Immortal Life of Henrietta Lacks brought Lacks’ story into the mainstream, the foundation provides financial assistance to people who were involved in historic scientific research without their knowledge, consent or benefit and their descendants. The Foundation has given grants not only to Lacks’ descendants, but to family members of the unwitting participants in the Tuskegee syphilis studies and the human radiation experiments, among others.
In August last year, UK based firm Abcam became the first ever biotechnology company to make a donation to the Henrietta Lacks Foundation that has used HeLa cells in its research. This was followed by an undisclosed six-figure donation to from the Howard Hughes Medical Institute (HHMI) in October, the largest non-profit biomedical research institution in the US. Alongside HHMI, National Institutes of Health director Dr Francis Collins has donated a portion of his 2020 Templeton Prize to the foundation.
In a statement made at the time, HHMI president Erin O’Shea said: “Scientists at HHMI and across the life sciences have made breakthroughs using HeLa cells, and we want to recognise the great benefit to science that Henrietta Lacks made possible. In the wake of recent, highly visible racist events, HHMI’s community has come together to set new goals for diversity, equity and inclusion.”
The reparative donations to the foundation have reignited conversations about informed consent when it comes to medical research. Current US regulations mean informed consent is only required for specimens that are considered ‘identifiable’, under Common Rule regulations, which in practice means little more than that the specimens ought not to be named after them.
In the 1970s, a leukaemia patient named John Moore donated blood samples believing they would be used for diagnostic purposes. Instead, the material was cultured into a cell line that became part of a patent application. Moore initiated legal action, but when the case was heard in front of the California Supreme Court, it ruled that a person’s discarded tissue does not qualify as their own personal property.
Under US law, a person’s cells can be used to make billions, of which they’re not owed a penny.
Seeking informed consent is easier said than done
Collins has indicated that he wants the research community to consider altering the Common Rule, so that consent is required from anybody from whom specimens are taken before said specimens can be used in any clinical studies.
But many researchers have warned that amending the Common Rule in this way could create undue burden for scientists, particularly when it comes to cell lines like the HeLa cells.
“I do think that if any sort of economic benefit comes directly from a person’s piece of tissue that they should have some sort of stake in that, particularly if it leads to a pharmaceutical product or a diagnostic,” says Kroll.
“The counter-argument is that it’s very difficult to keep track of what contribution a particular piece of tissue has made to a larger piece of intellectual property. There are many companies that sell intellectual property inside of a HeLa cell. If you’re a researcher purchasing a $10,000 HeLa cell line, that has in it a whole bunch of machinery that was created by someone else’s intellectual invention, what percentage of that price is because of HeLa cells and what percentage of that is the seller’s intellectual property?”
Even if researchers were to try and seek informed consent when building future human cell lines, they are often taken from exceptionally aggressive tumours like Lacks’. Because they must be preserved and cultured as soon as possible, the window to try and obtain informed consent from a patient is incredibly slim. If the cells perish in a petri dish before the patient can sign on the dotted line, the potential for vital scientific discovery could be lost.
There’s also the more troubling question of whether informed consent is worth the potential benefits of medical research. If a person’s cell sample can be used to save millions of lives, should they be given the opportunity to say no to the research?
We know that right cell line can change the course of history – it’s impossible to say where we’d be today as a species without HeLa cells, but there’s every chance we’d be far worse off.
There may never be another discovery like HeLa cells
However, it’s unlikely there will ever be another cell line quite as remarkable as HeLa cells.
“It’s very hard for any one person’s particular tissue donation to be used for a product anymore,” says Kroll. “There highly publicised cases are more the exception than the rule.
“Usually, your tissues are pulled together with hundreds of thousands of other specimens to look at a broad base of people of a certain demographic to look for disease risk or diagnostic criteria. It’s very rare your own cells lead to a blockbuster scientific discovery.”
Perhaps what is most crucial here is not how best to regulate potential future discoveries, but how to make amends to people wronged by historic ones. The killing of George Floyd and the ensuing Black Lives Matter protests in 2020 have prompted many medical institutions to examine how their work builds on racial injustice, and how best to atone for the way their work has profited from this damage.
For the scientific industry to thrive on HeLa cells while Lacks’ descendants could barely afford to get by is a blatant, longstanding injustice rooted in racism. Racial disparities in healthcare aren’t something that’s going away, especially as the Covid-19 pandemic continues to disproportionately impact Black Americans while HeLa cells are utilised as a vital part of vaccine research.
“It’s really a travesty that our system works this way,” says Kroll. “Our Foundation is really set up to remedy that situation for this group of people, under the umbrella of the Henrietta Lacks story as an example of why these disparities exist.”



