One of the ten most common cancers globally, pancreatic cancer caused over 430,000 deaths in 2018 with the five-year survival rate type standing at only 9%, compared to 87% for breast cancer in the UK.
A recent piece in the World Journal of Oncology described pancreatic cancer as one of the most lethal malignant tumour types. There is a range of explanations for this, including issues with diagnosis as patients do not exhibit symptoms at the early stages of the disease and a lack of treatment options.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Launched in 2011 in the UK, Pancreatic Cancer Awareness Month is now held globally every November with the aim of a rectifying this situation and demanding better for those affected by pancreatic cancer.
Pancreatic cancer’s rejection of immunotherapies
First conceived in the late 19th century by William B Coley and re-focused on in the 1950s, immunotherapy is now a staple of oncology treatments across a range of tumour types. It has allowed patients effective alternatives to surgery, as well as toxic chemotherapy and radiation therapy.
However, this approach of harnessing the immune system against cancer cells has struggled against pancreatic tumours. Although chemotherapy is effective in some patients, particularly those with resectable disease, according to an article in Annals of Gastroenterological Surgery journal, there have been limited treatment innovations since the late 1990s.
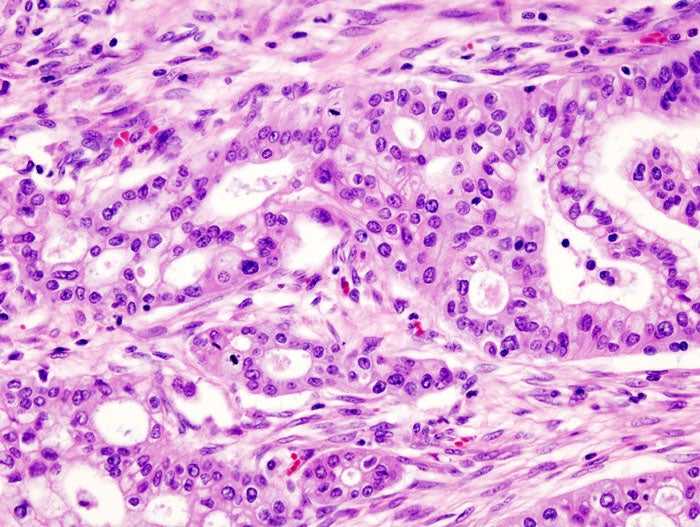
Pancreatic cancer patients have not responded well to immunotherapies targeting checkpoint inhibitors programme cell death 1 (PD-1) and cytotoxic T-lymphocyte, associated antigen 4 (CTLA-4), which have been effective in other cancers.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataIt is thought this is because pancreatic cancers are non-immunogenic and have poor antigenicity, compared to melanoma and lung cancers, which have responded particularly well to anti-PD-1 drugs like Merck’s Keytruda and Bristol-Myers Squibb’s Opdivo.
Identifying immune cells responsive to pancreatic cancer
Researchers from the University of Minnesota led by immunologist Ingunn Stromnes discovered a population of certain, rare T cells that can recognise, and then attack, pancreatic cancer cells, thereby suggesting that the presence of these rare T cells in some patients improved the effectiveness of immunotherapy approaches in pancreatic cancer patients.
With grant money from the Pancreatic Cancer Action Network, Stromnes’s team carried out animal studies to study the efficacy of neoantigen-specific T cells, combined with a combination PD-ligand 1 to block the tumour’s ability to defend itself against an immune attack. Results were published in the Cell journal in August this year.
Stromnes noted: “Our results must be interpreted with caution, because all the studies are in animal models. However, they do support testing this immunotherapy combination in clinical trials, at least in patients that have these rare T-cells.
“The next step in the lab is to identify the molecular traits of these tumour-reactive T-cells that are capable of effectively killing pancreatic cancer in animals.
“With this understanding, we hope to develop more effective cellular therapies for targeting this disease and to identify other rare T-cells that can recognize pancreatic cancer in patients.”
Developing therapeutic vaccines to spur immune response
Another approach to improve how the immune system fights cancer is John Hopkins Medical School’s pancreatic cancer vaccine, which aims to treat rather than prevent the condition.
The vaccine contains inactivated pancreatic cancer cells, which are incapable of dividing, and modified to release a certain molecule to attract T cells to cancer cells. Ultimately, the aim of the vaccine is to transform a non-immunogenic tumour into an immunogenic one, as stated in a 2014 article in the Cancer Immunotherapy Research journal.
Importantly, the vaccine will trigger T cells to attack pancreatic cancer cells wherever they have spread in the body, therefore potentially meeting the unmet need in systemic types of pancreatic cancer.
The vaccine, developed by medical oncologist Lei Zhang’s team, is currently being studied in clinical trials; there is significant optimism about its potential to improve pancreatic cancer treatments.




