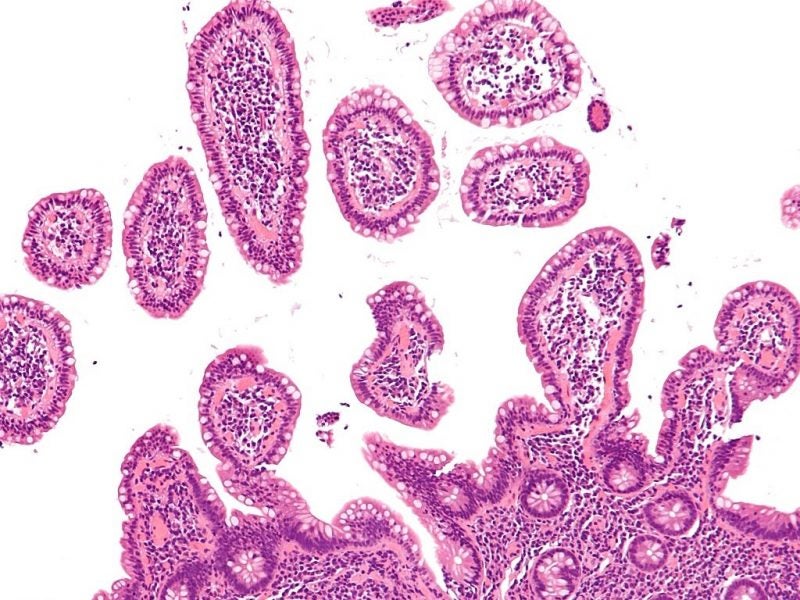
Affecting one million people globally, lymphoma is a type of blood cancer, specifically of white blood cells called lymphocytes; it causes them to become abnormal, meaning they cannot effectively fight infection, and causing them to form a tumorous lump. This form of cancer originates in the lymphatic system, allowing it to easily spread around the body.
To raise awareness of lymphoma symptoms, diagnosis and treatment, a global network of patient cancer groups called the Lymphoma Coalition marks World Lymphoma Awareness Day on 15 September every year. This awareness day occurs within World Leukaemia and Lymphoma Awareness Month.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
Lymphoma differs from leukaemia, which is another cancer of white blood cells; in the latter abnormal cells develop and build up in the bone marrow or blood stream, rather than the lymph nodes.
Many treatments have been developed for lymphoma and the majority of people survive the condition – the five-year survival rate of non-Hodgkin lymphoma, the most common type, is 70%, according to the US National Cancer Institute. However, it is common for lymphoma cells to become resistant to existing therapies, particularly chemotherapy, creating a new unmet need in lymphoma.
Understanding lymphoma’s tendency towards drug resistance
Genetic factors were traditionally assumed to be responsible for drug resistance; however, researchers are beginning to debunk this theory and move towards fully understanding lymphoma’s mechanism of drug resistance.
Using resistant model cell lines, researchers from the Moffit Cancer Center and Dana-Farber Cancer Institute discovered that resistance to the drug venetoclax in B-cell lymphomas was dependent on both genetic mutations and other mechanisms.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe venetoclax-resistant cells had an amplification of part of chromosome 18, which contains the BCL-2 gene; BCL-2 is venetoclax’s target to overcome the de-regulation that causes haematologic malignancies. However, transcriptional reprogramming dependent on the CDK7 protein was also present in the resistant cells, but not in the comparator non-resistant cell lines.
Co-lead researcher Jinaguo Tao from the Moffit Cancer Center’s department of laboratory medicine and haemoatopathology explained: “Certain regions of the DNA called super-enhancers became activated or deactivated in the resistant cells, leading to either a downstream loss or gain in protein expression, which ultimately contributed to cell survival.
“The study, for the first time, unified genetic alteration and non-genetic adaptive response as a driving force for drug resistance evolution to therapy.”
Resolving treatment resistance in lymphoma
Linked to their research focusing on understanding resistance, the Dana-Farber and Moffit researchers used their findings about the CDK7-based mechanism of resistance to develop a treatment strategy to overcome resistance.
They found that combining Ventoclax with CDK7-targetting inhibitor THZ1 prevented the emergence and maintenance of resistance to Ventoclax in cell models of two B-cell lymphomas, mantle cell lymphoma (MCL) and double-hit lymphoma. The results suggest that transcription-targeting agents could offer a new method to disable drug resistance in B-cell lymphomas.
Dana-Farber Cancer Institute and Harvard Medical School Department of Cancer Biology assistant professor in medicine Jun Qi commented: “Disabling CDK7 in combination with ABT-199 is an attractive means to provoke tumour regression of otherwise refractory lymphoma, and such a combination strategy could be applied across a broad spectrum of hematological malignancies.”
Discovering drugs for ibrutinib resistance in MCL
Additionally, a team from the University of Texas MD Anderson Cancer Center identified a small molecule, which could be effective in MCL patients who are resistant to Imbruvia (ibrutinib). One year survival rate of MCL after relapse on ibrutinib is 22%.
The drug in question is IACS-10759 and it was discovered by MD Anderson’s Therapeutics Discovery division, which focuses on drug discovery for unmet needs.
Researchers studied the link between metabolic reprogramming focused on glycolysis and oxidative phosphorylation (OXPHOS) and cancer cell growth in three patient-derived xenograft mouse models, as well as using genomic analysis of the specimens.
Study lead and MD Anderson professor of lymphoma & myeloma Michael Wang explained: “To investigate the therapeutic effects of IACS-10759, we developed an ibrutinib-resistant B-cell lymphoma mouse model using tumour cells isolated from cerebrospinal fluid from a patient who did not respond to multiple therapies including ibrutinib.
“We showed that metabolic reprogramming toward OXPHOS and glutaminolysis is associated with therapeutic resistance to ibrutinib in MCL, an incurable B-cell lymphoma with poor clinical outcomes.
“Inhibition of OXPHOS with IACS-10759 results in marked growth inhibition in vivo and in vitro in ibrutinib-resistant, patient-derived cancer models.”
The team is continuing its research into IACS-10759 in MCL patients, and MD Anderson’s Phase I trial will include an ibrutinib-resistant cohort.




