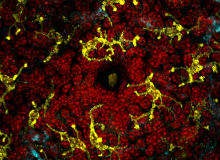

In recent years, the human microbiota has attracted attention as one of the most intriguing and underexplored areas of medical research. Referring to the 100 trillion or so bacteria that inhabit the human gut – which together comprise around 1-3% of a person’s body weight – the microbiota exists in a largely symbiotic relationship with its human host. For instance, certain bacterial species enable digestion, breaking down nutrients that humans would otherwise struggle to metabolise.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
While much remains unknown, scientists are beginning to look hard into the ways gut bacteria can help and harm human health. The Human Microbiome Project, completed in 2013, provided genome sequencing of the microbiota, allowing researchers to understand exactly which micro-organisms are present and what genetic material they contain.
As more is learnt, there has been a growing buzz around the idea that gut bacteria comprise a kind of ‘second genome’, with each person’s distinct microbial makeup wielding its own particular influence. The microbiota is now thought to play a role in everything from obesity to susceptibility to infection.
"At this point, we are only just beginning to appreciate how the microbiota affects our normal physiology," explains Matthew Redinbo, a professor of chemistry at the University of North Carolina at Chapel Hill. "That has been like knowing that there is a vast extra organ in the human body, but that it contains functions we cannot see or understand. With an increasing appreciation of the detailed actions played by the microbiome, we can begin to treat microbial factors like we treat human ones – as potential bona fide drug targets. That will represent a new paradigm in drug development."
An alternative to antibiotics
In 2010, Redinbo conducted pioneering studies in mice, which hinted towards the possibilities that may lie ahead. He found that, through manipulating the microbiome (i.e., the genetic material contained within the gut bacteria), it was possible to reduce the debilitating side effects associated with the cancer drug irinotecan.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataA standard treatment for colorectal and pancreatic cancers, irinotecan needs to be limited in dose because of its gastrointestinal toxicity. Despite having one of the highest rates of diarrhea of any chemotherapeutic agent, the drug currently has no therapeutic adjunct that could be used to mitigate these effects. Redinbo showed that, through inhibiting certain bacterial enzymes, the GI disturbance was lessened.
"We showed that the microbiome contained therapeutic drug targets that could be modulated with pharmacological compounds toward improving the treatment of disease," he explains. "We also established, and met, clear criteria for success – compounds needed to be potent, selective and non-lethal. Selectivity was crucial toward microbial enzymes relative to their mammalian counterparts. Non-lethality was also critical; all current drugs that target bacteria are antibiotics."
Antibiotics may sound like a good idea on the face of things, insofar as they kill the bacteria that cause the effects. However, it can unbalance the complex ecosystem within the gut and increase the spread of so-called ‘bad bacteria’. This applies above all to patients with compromised immune systems, such as those who are undergoing chemotherapy.
Redinbo’s strategy is different: it neither harms the bacteria nor targets biochemical processes in human cells. Rather, it targets the ways that pharmaceuticals interact with the microbiome, thus altering drug metabolism for the patient’s benefit.
Setting up trials
In the years since the completion of the mouse studies, he has co-founded Symberix, a biotechnology company that aims to take drugs of this kind to market.
"Symberix recognises the importance of both human health and microbiome health. We aim to discover and develop drugs that correct a disease-causing component of microbiome activity without killing its vast populations of beneficial bacteria. We can think of no existing medicines that work this way," explains co-founder, president and CEO Ward Peterson.
Efforts to develop this pharmaceutical are now well underway. Currently in the ‘lead optimisation’ phase, the programme will focus initially on irinotecan-induced diarrhoea, before looking at chemotherapy-induced diarrhoea more broadly. The goal is to identify a clinical candidate within the next year, before initiating investigational new drug-enabling activities and beginning clinical trials by the end of 2017.
Symberix also has a second programme in the works, which explores lower GI toxicities (enteropathies) associated with non-steroidal anti-inflammatory drugs (NSAIDs). These enteropathies, which can manifest as intestinal ulceration and inflammation, blood loss, anaemia and lower GI bleeding, can pose a serious problem for NSAID users. The company is hoping to find a clinical candidate in twelve to 15 months’ time and start clinical trials by early 2018.
"The therapeutic adjuncts used for CID and NSAID-enteropathies will need to be different drugs because of the patient population and differences in use of chemotherapy versus NSAIDs. Our goal is to develop therapeutic adjuncts that are optimised and tailored for the intended patient population," explains Peterson.
Opportunities ahead
As the programmes in question gather pace, it’s important to remember that this technology is unprecedented, facing challenges and opportunities alike.
"One question that comes to mind has to do with traditional drug discovery approaches used for human genome targets — how well do these approaches work for microbiome targets, for which there is no precedent?" says Peterson. " Another unprecedented aspect of Symberix is that there are no approved products for the two lead indications CID and NSAID-enteropathy. Thus, there is no established regulatory pathway and no existing market."
As he sees it, the lack of prior examples gives Symberix a great chance to pave a regulatory pathway, bringing important products into untapped and under-served markets, and ensuring that existing treatments don’t create more problems than they solve.




