by Manasi Vaidya in New York
OncoSec Medical’s tavokinogene telseplasmid’s (TAVO’s) potential in triple-negative breast cancer (TNBC) relies on ironing out operability unknowns, experts said. However, local administration in combination with SOC has piqued some interest.
Since distant metastases add a significant disease burden in metastatic TNBC, the impact of local intratumoral administration of TAVO on those metastases will be important, but is yet unknown. While early data indicated one response in such a case, the impact of TAVO’s administration in the primary tumor or metastases is unknown, experts added.
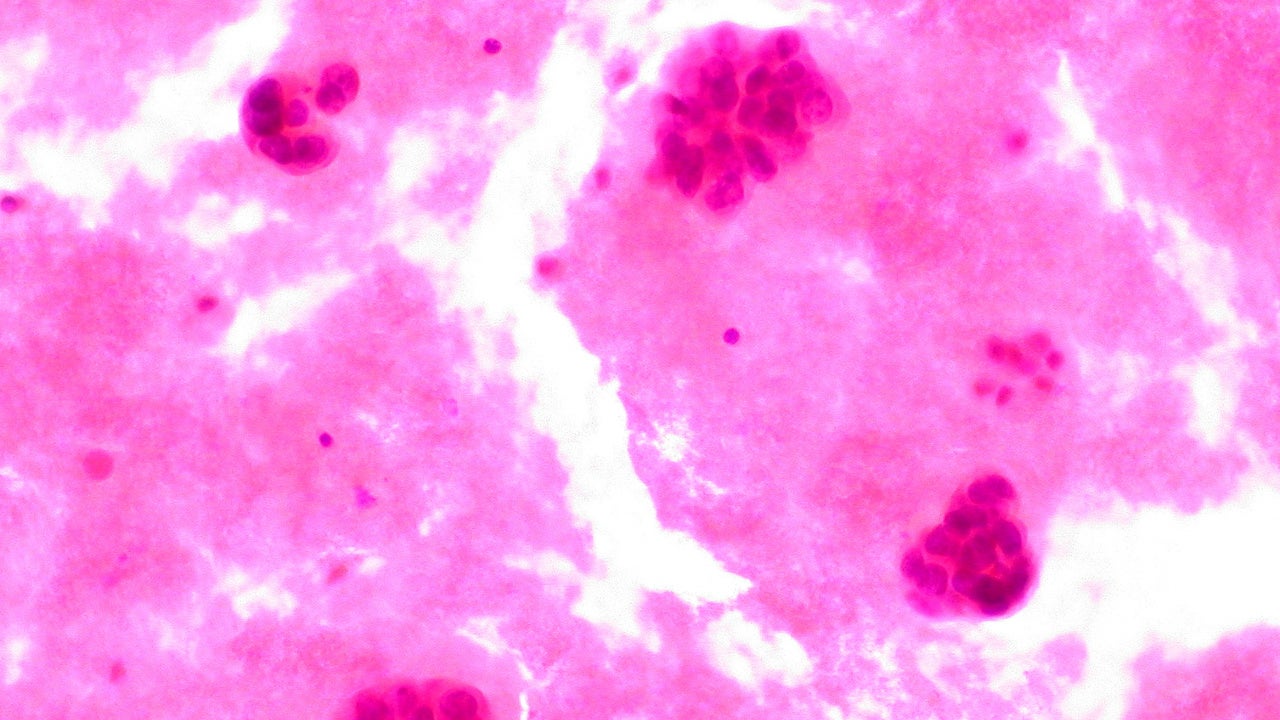
TAVO is a plasmid-based interleukin (IL)-12 to be administered locally at the tumor site using OncoSec’s electroporation device. Using the device in TNBC is feasible since breast tumors can be palpable, experts said, but one added this may be limited to superficial accessible tumors. Still, while the electroporation device used to deliver TAVO is innovative, it is not available outside clinical studies and requires specialized training to operate, limiting its use to only a few experts. Nonetheless, given IL-12’s immunostimulatory activity, there is strong scientific rationale to support its local intratumoral administration with a systemically delivered checkpoint inhibitor, experts said. The early Phase II efficacy TAVO data in combination with Merck’s Keytruda (pembrolizumab) was significant given the low responses seen with Keytruda alone in the pretreated setting, experts said.
The Phase II KEYNOTE-890 study (NCT03567720) is enrolling 40 patients who will receive TAVO plus Keytruda/chemotherapy in the first-line setting. If successful, this cohort will expand to a registrational study, as per a November company presentation. One analyst noted KEYNOTE-890 is important since Keytruda has moved into first-line metastatic TNBC. On 13 November, the FDA approved the Keytruda/chemotherapy combination in the first-line setting for metastatic TNBC patients whose tumors are programmed death-ligand 1 (PD-L1) positive. If the trial emerges with improved responses, that would be a significant event for OncoSec, said the same analyst.
OncoSec’s market cap is $186.14m. OncoSec declined to comment on this article.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataAppropriate cancer model, delivery method distinct
Breast cancer lends itself well to this approach, as other tumors may be located in deep-seated locations requiring an interventional radiologist to access, said investigator Dr Melinda Telli, associate professor of Medicine, Division of Medical Oncology, Stanford University School of Medicine, California. In breast cancer, the tumor is often palpable, she said, adding the electroporation procedure does not require an operating room or take too long.
Electroporation destabilizes the cell membrane, making the cell take up the plasmid-encoding IL-12, resulting in the local expression of the cytokine, according to OncoSec. The electroporation device’s applicator needle only extends to 1.5cm, so the tumor cannot be very deep beneath the skin, Dr Anthony Olszanski, chief, Section of Solid Tumor Oncology, Fox Chase Cancer Center, Philadelphia, Pennsylvania. The device’s use may be limited to more superficial tumors, but technology can be further developed to improve on this, he said. Locally administering the drug in truly visceral lesions is not a problem, but with axillary tumors or those in sensitive areas it can be uncomfortable for patients, said Olszanski. Patients can be given narcotics for pain control, he added.
However, electroporation is rarely used in the clinic, and research with this administration route is still limited and nonstandardized, said David Stepensky PhD, associate professor, Department of Clinical Biochemistry and Pharmacology, Ben-Gurion University of the Negev, Israel. Special training is required to use the electroporation device, said Olszanski, addeding this approach can carve out a space for itself in the treatment landscape like Amgen’s Imlygic (talimogene laherparepvec). Similar to TAVO, Imlygic also relies on an intratumoral administration, but is given by an injection into cutaneous, subcutaneous, and/or nodal lesions in metastatic melanoma. While the electroporation concept could be effective, it is still early to make such a prediction, agreed Dr William Carson, associate director for Clinical Research, OSU Comprehensive Cancer Center, Columbus, Ohio. There is some promise for local administration providing better efficacy, but there has been a clear gap between expectations and performance thus far, said Stepensky.
A local intratumoral approach holds appeal in terms of the MOA, said experts. The potential to directly change the tumor microenvironment (TMI) with IL-12 and pointedly target the tumor could lead to robust efficacy with fewer adverse events, said Olszanski and Carson. Also, IL-12 is a strong stimulant for T cells and natural killer cells, and its potential to stimulate the immune system has been studied in several preclinical and clinical oncology trials, said Carson. This is significant, since while checkpoint inhibitor/chemotherapy combinations are approved for PD-L1+ metastatic TNBC patients, about 60% of patients do not express PD-L1 at a high enough level to derive benefit, Telli added. Carson likened the IL-12 approach to hitting the accelerator while checkpoint inhibitors would take the brake off immune checkpoints.
TAVO addresses a challenge with other administration modes where a cytokine like IL-12 is cleared too quickly before it can kick off a proinflammatory cascade, said Telli. The TAVO plasmid may lead to sustained local production; if it is maintained long enough, it will allow immunological changes in the TMI, she added.
The Phase II TAVO data is still early, but its efficacy potential is nonetheless encouraging, said experts. As per a San Antonio Breast Cancer Symposium (SABCS) 2019 abstract, of the 11 evaluable patients treated with TAVO/Keytruda in the ongoing Phase II study, three had a partial response (PR), including one with multiple metastases and a short disease-free interval following neoadjuvant chemotherapy, bringing the ORR to 27.3% (P3-09-04). The patients in the initial cohort were heavily pretreated where the responses were likely to be low, which makes the ORR impressive, said Telli. Carson also found the response data exciting, but retained caution for future results due to the limited Phase II data. The observed responses were only partial, which makes it difficult to correlate the efficacy with the IL-12 delivered by TAVO or eliminate a chance result, said Stepensky. Furthermore, there is no randomized control arm yet, he added.
Impact on distant metastases unknown
While technically feasible, a major question with a TAVO-like approach is whether it will subsequently generate a systemic response, said a breast cancer oncologist. The Phase II study is specifically enrolling patients with inoperable locally advanced or metastatic TNBC.
TNBC is associated with potentially life-threatening visceral metastases, so for local therapies to be beneficial, they need to engender a systemic immunological response, said the oncologist. However, the ability to stimulate an immunological response at metastatic sites is limited, said Stepensky. While no impact on distant metastases was observed with TAVO, Carson did not dismiss the therapy’s potential. There can be situations where the primary tumor shrinks due to therapy, which could allow for surgery or chemotherapy for long-term beneficial effects, he said.
Once the primary tumor is injected with a drug, positive effects on noninjected cutaneous, nodal or visceral lesions do happen, although at a lower rate compared to what has been seen with Imlygic, said Olzasnski. The TMI is different in metastases compared to primary tumors, but an intratumoral approach can change the TMI and cause tumors to express new antigens for the immune system to attack, Olszanski added.
One unnamed Grade 3 or higher adverse event was observed with TAVO/Keytruda, but it was attributed to Keytruda. Usually smaller doses are given so the side-effects due to local IL-12 are not too severe, said Stepensky. Systemic toxicity concerns are limited with local administration, said Stepensky. TAVO is well-tolerated, which is not the case with systemic therapies that breast cancer patients receive in this line of treatment, said Olszanski.
Manasi Vaidya is a Senior Reporter for Clinical Trials Arena parent company GlobalData’s investigative journalism team. A version of this article originally appeared on the Insights module of GlobalData’s Pharmaceutical Intelligence Center. To access more articles like this, visit GlobalData.