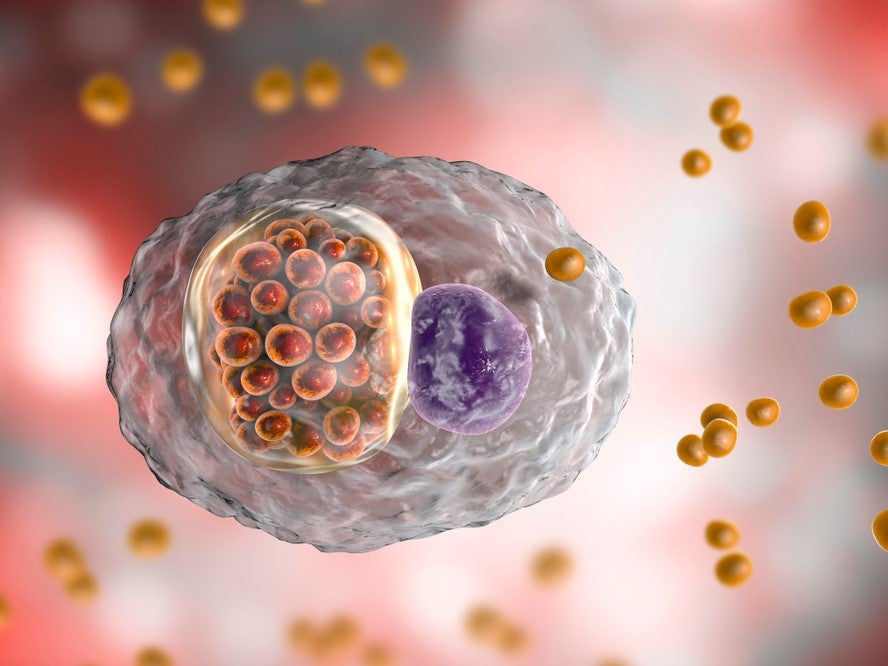
Chlamydia is the most common bacterial sexually transmitted infection (STI) in the world. The World Health Organization (WHO) estimates it affects around 131 million people globally each year.
Initially believed to be a viral disease, it was identified as being caused by the bacterium Chlamydia trachomatis soon after Alexander Fleming’s 1928 discovery of Penicillin, the first antibiotic, and this type of drug became widely used. Antibiotics quickly became the standard of care for chlamydia in the late 1930s and other bacterial-based STIs, such a syphilis and gonorrhoea.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
The two main antibiotics used against chlamydia are azithromycin and doxycycline; others on a WHO list are amoxicillin, erythromycin and tetracycline.
Although antibiotics have been shown to be highly effective at clearing Chlamydia trachomatis from patients, they are not perfect. This has pushed researchers to look at alternative treatment options for the most common STI, including a preventative vaccine and gene therapy.
Challenges in treating chlamydia
Chlamydia remains so common because of its asymptomatic nature, causing some people to be residual sources of infection. This makes it tricky to catch early and be treated with antibiotics, which is an issue since it causes serious diseases of the cervix, pelvis, testes and urethra.
One of the more serious complications of this STI is pelvic inflammatory disease; the CDC estimates it occurs between 10% and 15% of women with untreated chlamydia and can cause permanent damage to fallopian tubes and potentially fatal ectopic pregnancy.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataIn addition, recurrence of the disease is common – affecting approximately a quarter of patients, according to the US Center for Disease Control and Prevention (CDC) – leading to another course of antibiotics. This over-use of antibiotics, combined with patient misuse or nonadherence to prescribed medications, has caused the emergence of antimicrobial resistant (AMR) strains of Chlamydia trachomatis.
This has left patients with a situation where the treatments used against the condition, although effective, are not fit for purpose to end reduce the rate of chlamydia infections and its co-morbidities.
A WHO STI 2016 guidance document explicitly stated “there is an urgent need to update global treatment recommendations to effectively respond to the changing AMR patterns of STIs” and “therapeutics, vaccines and barrier methods offer better opportunities for the prevention and care of STIs.”
Beyond antibiotics towards preventative vaccines
Vaccines have been shown to be successful at drastically curbing infection rates – they are responsible for the eradication of ; for example, widespread vaccination of girls aged 12 and 13 against human papillomavirus (HPV) was recently shown by a Canadian study to significantly reduce the prevalence of genital and cervical cancer-causing strains of the virus.
“The success of the HPV vaccines has shown us how effective vaccination can be against a sexually transmitted infection” encouraged researchers from Statens Serum Institut (SSI), Denmark, and Imperial College London to develop a preventative vaccine for chlamydia, SSI Department of Infectious Disease Immunology director Frank Follman explains.
Imperial College London Department of Infectious Disease Mucosal Infection and Immunity unit head Professor Robin Shattock noted: “It [chlamydia] is very treatable if identified, but as many people don’t have symptoms it can be missed.
“One of the problems we see with current efforts to treat chlamydia is that despite a very big screening, test and treat programme, people get repeatedly re-infected. If you could introduce a protective vaccine, you could break that cycle.”
After 15 years of research, involving discovering a weakness in chlamydia to target, the UK-Danish team recently published results from the first human trials of two versions of their vaccine. Both forms of the vaccine targeted the recombinant protein subunit CTH522 – one was modified with CAF01 liposomes, the other with aluminium hydroxide.
Promising immune response from chlamydia vaccine
The two versions of the vaccines were well tolerated and immunogenic; no participants of the placebo group achieved an immune response.
Shattock commented: “The findings are encouraging as they show the vaccine is safe and produces the type of immune response that could potentially protect against chlamydia.” Folmann explains the reason for its success was the vaccine’s “combination of neutralizing antibodies and T cells”.
“The most important result is that we have seen protective antibodies against Chlamydia in the genital tracts. Local immunity in the genital tract is important to stop the infection as quickly as possible” Follmann added in a statement. This will help to generate a long term immune response against the bacterial condition.
Due to the vaccine’s success, the researchers are planning to move into further clinical trials to find out “whether it is truly protective or not”, Shattock explained. It is likely that the more effective of the two, the CTH522 vaccine adjuvanted with CAF01 liposomes, will become the primary focus of future trials.
In the long term, the researchers are considering combining their chlamydia vaccine with the successful HPV vaccine “in the same target population,” to further prevent severe consequences these STIs can have on women’s health, notes Folmann.




