Researchers at the US National Institutes of Health (NIH) unit National Eye Institute (NEI) have identified two potential drug candidates for age-related macular degeneration (AMD) treatment.
The drug candidates were identified using a stem-cell-based research tool.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.
A main cause of blindness, AMD has no therapy available so far.
Leveraging the stem-cell-derived model, the scientists monitored the drugs to analyse whether they could slow or stop AMD progression.
Findings showed that these drugs could potentially avert key phenotype development in the model.
These phenotypes include drusen build-up, lipid-rich accumulation in the retina and the retinal pigment epithelium (RPE) cells atrophy or shrinkage.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
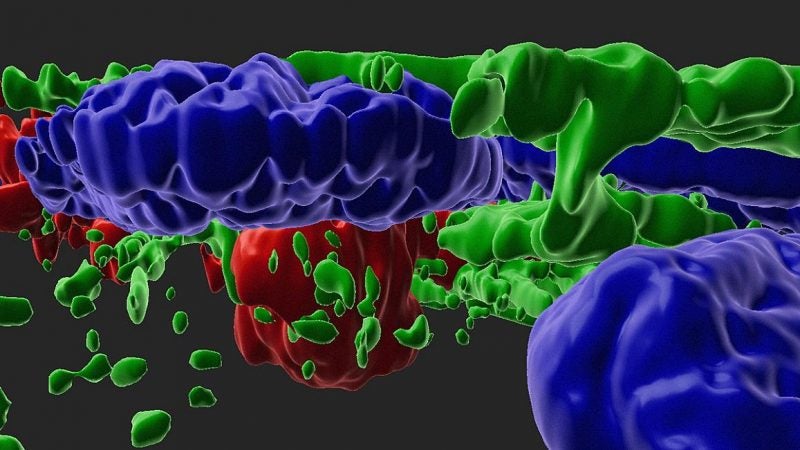
By GlobalDataThe light-sensing photoreceptors of the retina are nourished by a layer of tissue called RPE.
In AMD patients, RPE cells contract and die. RPE deficiency causes photoreceptor death, which results in vision loss.
NIH noted that the study findings show how genetic variants can impact the development of AMD.
In prior genetic studies, some individuals with AMD had mutations in genes that control the alternative complement pathway, a key element of the immune system.
However, the exact mechanism by which the genetic variants cause AMD was not known.
The scientists exposed ten iPSC-derived cells to anaphylatoxins from human serum.
They used the model to analyse more than 1,200 drugs and found that two drugs demonstrated the ability to hinder RPE atrophy and drusen formation.
Of the two drugs identified, L745 was found to be more promising. It was developed by Merck & Co and initially analysed to treat schizophrenia.
NEI director Michael Chiang said: “This stem-cell-derived model of dry AMD is a game-changer.
“Scientists have struggled to unravel this incredibly complex disease and this model could prove to be invaluable for understanding the causes of AMD and discovering new therapies.”
Last month, researchers from NIH unit National Institute on Ageing (NIA) found that present and developing cancer therapies could be repurposed for Alzheimer’s treatment.




