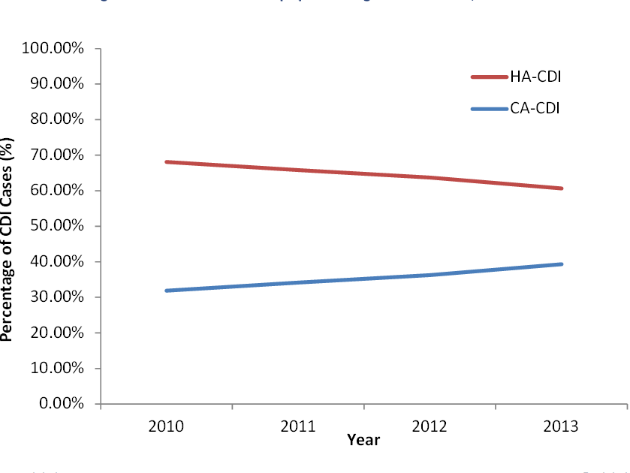
The percentage of clostridium difficile infections (CDI) in the US that originate outside of healthcare settings has been growing in recent years. Data from the Center for Disease Control and Prevention’s Emerging Infections Program (EIP) shows that community-associated CDI (CA-CDI) cases are increasing at a faster rate than healthcare-associated CDI (HA-CDI) cases.
Between 2010 and 2013, CA-CDI grew from 31.87% of CDI cases to 39.32%. Figure 1 displays the steady relative growth of CA-CDI in the US in these years.

Discover B2B Marketing That Performs
Combine business intelligence and editorial excellence to reach engaged professionals across 36 leading media platforms.

CDI is primarily transmitted through the fecal-oral route. The typical clinical symptoms of CDI include watery diarrhea, anorexia, and nausea, as well as hypoalbuminemia and abdominal tenderness in severe cases. The EIP estimated that there were 469,200 CDI cases in the US in 2013.
The primary risk factor for CDI is treatment with antibiotics, with varying risks depending on the antibiotic used. After antibiotics kill off the normal, healthy gut bacteria, C. difficile takes over the gut and can cause potentially serious infections.
Historically, CDI has been considered a predominantly hospital-acquired infection. However, trends since 2010 suggest that the number of CA-CDI cases may soon approach the number of HA-CDI cases. These changes could be the result of increases in antibiotic consumption or exposure to C. difficile in outpatient settings. However, recent studies have reported CA-CDI cases in people without recent antibiotic use or healthcare exposure.

US Tariffs are shifting - will you react or anticipate?
Don’t let policy changes catch you off guard. Stay proactive with real-time data and expert analysis.
By GlobalDataThe changing epidemiology of CDI warrants sustained awareness of the situation and preventative measures. This includes careful monitoring of antibiotic prescribing patterns, improved infection control in outpatient settings and surveillance of community-acquired infections.
Details about the trend analysis and other discussions of CDI epidemiology can be found in the upcoming EpiCast Report: Clostridium difficile Infection (CDI) – Epidemiology Forecast to 2026 and EpiCast Model: Clostridium difficile Infection (CDI) – Epidemiology Forecast to 2026.


