
Clinical trials are producing more data than ever before, drawing from vast and diverse datasets that must be cleaned and reconciled under tight timelines. While data volume and complexity continue to grow, many organisations still rely on fragmented tools and manual processes to manage them.
This misalignment is creating pressure across clinical data management teams, with manual data cleaning being time-consuming and resource-intensive. Trial timelines, budgets, and regulatory submissions can all be impacted. Consequently, platform-based approaches to data management are emerging as a practical solution, bringing data, workflows, and oversight into a single, integrated system.
Cleaning clinical trial data: The challenges
One of the most persistent challenges in clinical data management is the work required to clean and reconcile data. As trials become more complex, data managers must contend not only with increasing volume but also with variation in format, structure, and source.
Each additional system introduces new discrepancies, queries, and points of failure. Manual data cleaning amplifies these challenges, including tasks such as identifying inconsistencies, generating queries, reconciling datasets, and tracking resolutions that rely on spreadsheets, emails, and multiple disconnected tools.
The impact of these inefficiencies can lead to delays in data cleaning, which in turn pushes back interim analyses and regulatory submissions. The result is an increase in overall trial costs and an extension of the time to market. In competitive therapeutic areas, even small delays can have significant commercial and patient-care implications.
Fragmentation across systems and teams in clinical trial data
Another obstacle is the lack of integration across clinical systems. Data is often spread over EDC platforms, laboratory information systems, safety databases, and external vendor tools. Each system may operate with its own data standards, workflows, and access controls, requiring manual hand-offs and reconciliation at multiple stages.
This fragmentation affects collaboration, with clinical data managers, statisticians, clinical operations teams, and external partners frequently working in parallel but lacking a shared, real-time view of data quality and progress. As a result, issues may be identified late, duplicated across teams, or resolved inconsistently.
From a governance perspective, fragmented systems also make it more difficult to maintain auditability and oversight. Tracking who made changes, when they occurred, and why they were necessary can become complex, increasing compliance risk and adding pressure during inspections and audits.
Historically, many organisations have addressed data management challenges by layering additional point solutions onto existing infrastructure – such as query management tools or data reconciliation systems. While these tools may solve specific problems, they often introduce new silos and integration challenges that create further operational complexities.
Data managers must move between systems, re-enter information, and manually align outputs. Furthermore, training requirements grow, maintenance costs rise, and the risk of errors increases.
Rethinking data management as an integrated platform
Platform-based data management solutions take a fundamentally different approach. Rather than addressing individual pain points in isolation, they are designed to centralise data, workflows, and oversight within a single environment. This unified architecture reduces fragmentation and enables more consistent, automated processes.
By integrating data from multiple sources, platforms can support automated cleaning and reconciliation rules, reducing reliance on manual intervention. This means that data quality issues can be detected earlier, prioritised intelligently, and resolved more efficiently. The result is that data managers spend less time on repetitive tasks and more focus on important decision-making.
Platforms also enhance visibility and collaboration, enabling stakeholders across functions to access a shared view of data status, queries, and progress in real-time. This transparency supports better coordination between teams and helps prevent bottlenecks late in the trial lifecycle.
Scalability is another key advantage of a platform approach, with standardised workflows and configurable rules making it easier to onboard new studies, vendors, or data types while maintaining consistency.
From a compliance perspective, platforms also offer built-in audit trails, role-based access controls, and standardised documentation. These features simplify inspection readiness and reduce the burden associated with demonstrating data integrity and process control. Rather than assembling evidence across multiple systems, teams can rely on a single source of truth.
Improving decision-making with data in the trial lifecycle
Cleaner data that is delivered earlier in the trial process enables more timely analyses and reduces uncertainty at critical milestones. For sponsors and CROs, this can translate into shorter timelines, lower costs, and improved trial outcomes.
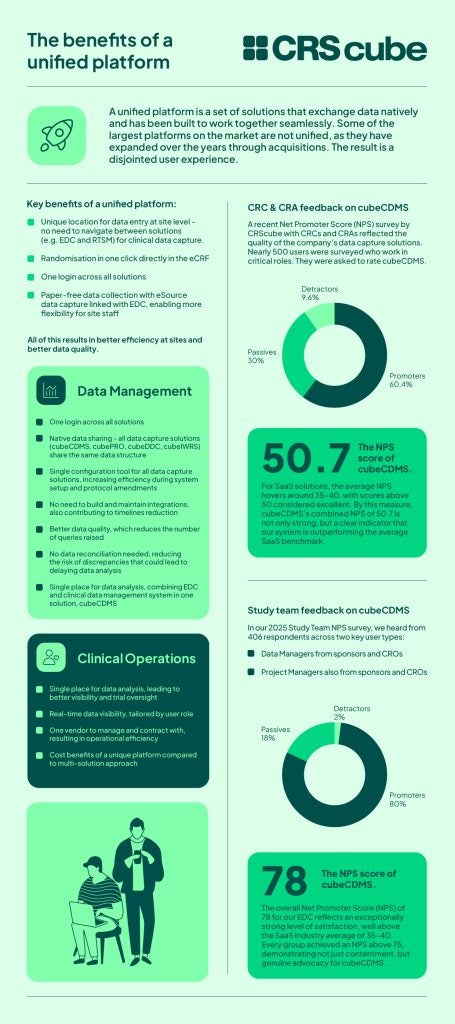
CRScube’s unified platform is an integrated approach to data management, with proven results. The CRScube suite is designed as a connected ecosystem of solutions that spans the clinical lifecycle, from electronic data capture and patient reporting through to trial management and risk-based quality oversight.
Because all CRScube solutions are built to share data and workflows natively, teams gain real-time visibility across functions without the need for costly custom integrations or error-prone hand-offs.
To learn more about CRScube’s suite of products and unified data management system, download the document below.



