Huma is a digital health company dedicated to digital-first care and research. It helps healthcare, biopharma and medical technology organisations to build SaMD solutions, bringing them to market on the back of Huma’s Class IIb EU MDR and Class 2 510k FDA regulated platform. Huma can also deploy AI models on its platform whether they have been developed in-house or by a customer.
We asked Jessica Cormier-Breslin, Huma’s Director of Clinical Services for US Healthcare; Michael Macdonnell, Global Head of Healthcare & Pharma Partnerships; and Benjamin Irving, head of Huma’s AI team, about Huma’s plans for Gen AI and how it fits into the SaMD sector.
Why has Huma invested in Gen AI?
Michael Macdonnell (MM): We were initially very interested in Gen AI as a way of improving our own productivity and the productivity of care. Gen AI is just one form of artificial intelligence. We do different types of algorithms which are about predicting risk. For instance, cardiovascular risks to help pre-screen people to make sure they get into services earlier. We also build algorithms that quantify or objectively measure symptoms, so you can see disease progression.
We have deployed Gen AI as well. We have built a partnership with Google, who are one of the leading providers with specific expertise in building models, trained on medical data, and medical literature.
How does Huma use AI to help clinical monitoring teams with their summaries?
Jessica Cormier-Breslin (JCB): AI is streamlining the process of patient monitoring by consolidating and summarizing data points, which can be overwhelming to sift through manually. Having AI assist in compiling these notes not only saves time but also ensures that critical information is readily accessible for clinical review. And it’s reassuring to know that there are multiple layers of human oversight in place to verify the accuracy and relevance of the information before it reaches the provider. This integration of AI with human expertise seems like a promising approach to enhancing healthcare efficiency while maintaining quality standards.
Can you give an example of where AI has given an insight to help clinicians make better decisions?
JCB: Imagine a patient with a history of respiratory issues, such as asthma or chronic obstructive pulmonary disease (COPD), who is being monitored using AI-assisted systems. The AI continuously collects and analyzes data from various sources, including patient-reported symptoms, vital signs, medication usage, and environmental factors.
Over the course of several days, the AI notices subtle changes in the patient’s respiratory symptoms, such as increased coughing or shortness of breath. While each individual change may not seem significant on its own, the AI recognizes a pattern emerging—a gradual worsening of respiratory function.
Additionally, the AI correlates this trend with other relevant data points, such as medication usage and environmental factors like air quality. It alerts the clinician to the fact that the patient has reported similar symptoms in the past and that their respiratory rate has been gradually increasing over the past few nights.
Based on this insight, the AI suggests that the clinician conduct a closer evaluation of the patient’s respiratory status. This is then escalated back to the provider and perhaps they order additional diagnostic tests, adjustments to medication dosages, or changes in treatment strategies.
In this scenario, the AI’s ability to detect subtle trends and patterns in the patient’s data allows clinicians to intervene earlier, potentially preventing exacerbations of the respiratory condition and improving overall patient outcomes. By augmenting clinical decision-making with data-driven insights, AI enhances the quality of care provided to patients with respiratory conditions.
What are the benefits of incorporating AI into Huma’s disease management platform? For example, can you take us through how Huma’s AI helps patients with myasthenia gravis?
MM: Our work on myasthenia gravis helps patients help themselves and gain insights into their own disease. Understanding their disease might be progressing or worsening with their clinical team on the other side to make decisions about that. For instance, ptosis is a symptom that you get in myasthenia gravis, (eyelid drooping) and you can see that because the camera will objectively quantify that it’s happening. You can make decisions earlier.
Benjamin Irving (BI): We leverage the smartphone as much as possible. We have voice metrics [using the] microphone, and we can quantify the presence of pitch and slurring. And we also utilise a camera so we have a fatigue test where we can track the patient and look at them performing different arm fatigue exercises, etc.
This is in the process of being integrated into the Huma platform. Then we’ll have a set of essentially quantitative measures that allows us to help the patient along the journey – looking at recovery improvement, undergoing therapy or if the condition is worsening, flag that to the clinician.
How does Huma use AI to improve patient engagement?
JCB: Huma leverages AI to enhance patient engagement through personalized messaging and communication. Clinicians can input the purpose of a message, and AI generates tailored notes that are more specific to each patient. This approach ensures that communications resonate with individuals across a wide range of ages and preferences, including those who may be less tech-savvy. Patients appreciate the sense of connection and support, knowing that there’s someone actively monitoring their health and available to address their concerns. This personalized approach fosters a stronger bond between patients and their care team, promoting better engagement and ultimately improving health outcomes. Patients have expressed gratitude when they realize there is an actual human monitor keeping an eye on them on the other side of the technology.
BI: Patients want the ability to track their disease. They only see a clinician every once in a while, so having these sort of AI tools that provide them with feedback, we expect that would improve patient engagement because they’re getting something back as part of the process.
How does Huma ensure the safe and responsible use of AI in healthcare?
BI: It’s not our data. So, we must be super conscious of that. We observe industry standards on privacy, security, etc. [Data] is not to be shared or sold to anybody.
JCB: [Some patients] love that their data is being stored in one place because they may have a specialist providing this service. For instance, they may be here for pulmonology, but they want to show [data] to their cardiologist. We have that data, and they can hit a download button and get their own data off [the app] so that they can provide it to other providers.
Overall, how do you see AI improving healthcare delivery in the next five years?
BI: One area is being able to provide quantification to the patients, measurements of condition quantification, so they can see improvement. There’s also a big area on leveraging the data that the patients input into the app for prediction of an exacerbation. Another is using AI to improve clinical workflows.
For instance, if you’re typing some notes, we can help with completion of those notes. Or prompting to speed up clinical management on that side. Of course, with AI comes data, so it’s also about what data you can integrate, and then build out those systems and test those systems.
MM: We are dedicated to implementing proactive care, rather than reactive. We’re trying to get to a point where we can use data much more frequently – using everyday data to empower people to look after themselves and give their clinical teams the information they need to diagnose and treat disease earlier.
AI in healthcare: GlobalData insight
Software as a Medical Device (SaMD) is software designed for medical purposes, providing additional capabilities and services to medical devices, and empowering patients to take control of their care, especially in areas with poor access to traditional healthcare.
Generative AI (Gen AI) refers to a category of deep-learning models that can generate high-quality text, images, and other content based on the data they were trained on.
AI can aid clinicians in their decision-making by providing insights from large data sets, including patient records, lab and pathology results, medical images, and data generated by mobile phones and wearable sensors. AI technologies can make ‘inferences’ or predictions from these data that can improve patient care, enhance diagnostic accuracy, streamline administrative tasks, and optimise healthcare delivery.
Some of the areas in which Gen AI can assist clinicians with includes:
- Identifying signs of disease or deterioration that prompt earlier diagnosis and clinical intervention
- Improving the accuracy of diagnostic imaging
- Increasing efficiency by reducing manual work and generating higher speed processes
- Helping to automate patient and healthcare professional communications, which can save time for healthcare professionals
- Providing clinical decision support to help promote guideline and data-driven care
- Helping improve the production of digital health technologies through automated software code generation
In the SaMD sector, Gen AI can improve personalised healthcare through the collection of patient data via wearable devices. Wearables provide continuous, real-time data, complementing traditional data sources such as imaging and patient records.
AI use in healthcare is set to increase as the technology evolves
According to GlobalData, AI is predicted to become a key driver of medical device innovation. The data and analytics company predicts that the use of AI within medical practices is likely to increase, with the AI market expected to grow from US$81 billion in 2022 to $909 billion by 2030[1].
Alexandra Murdoch, Medical Analyst at GlobalData, comments: “There are so many good uses for AI in the medical device industry. We know that it can be used for data management purposes, remote surgery, diagnostic and procedural assisting, clinical trials, and more.”
GlobalData has also classified AI as one of their major technology themes impacting the medical devices industry, along with cybersecurity, robotics, wearable tech, and cloud computing.
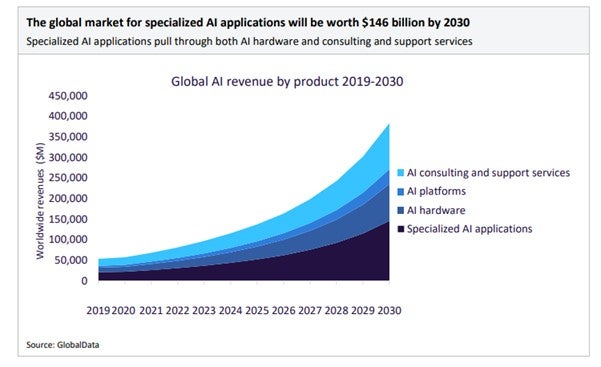
Source: GlobalData: Thematic Intelligence: Technology Artificial Intelligence, February 2023, page 20
While the integration of remote patient monitoring (RPM) in medical devices is relatively new, Covid-19 helped increase adoption rates significantly, with patients becoming more accepting of the technology. GlobalData predicts that RPM will continue to improve patient care, reduce hospital admissions, and facilitate early discharge, with the RPM market reaching $760 million by 2030.
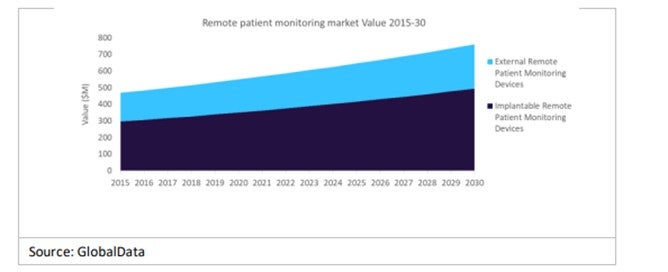
Source: GlobalData: Thematic Intelligence: Medical Device Predictions 2023, page 9
Further, GlobalData research shows that specialty mobile health apps, used with smartphones or tablets, will increase. Offering health features like step tracking, heart rate monitors, and sleep tracking, these apps are often used alongside wearable devices to remotely monitor patients with chronic diseases. These apps help manage therapies, monitor symptoms, and improve adherence to treatments.